VYONGWANI, KENYA – Mwaka Chimera sits on a worn-out leather couch outside her two-roomed house in Vyongwani village, in southeastern Kenya, cradling her newborn daughter.
“I dropped out of primary school, and for my first five pregnancies, I never attended a single antenatal clinic. I would just show up at the hospital when it was time to give birth,” Chimera, 31, says in Swahili. “The difference in how I’ve cared for my last two children is remarkable, all thanks to what I learned in the group.”
Through her local mother-to-mother support group, Chimera says she’s learned the importance of prenatal checkups and key screenings, including HIV testing. The group was part of Stawisha Pwani, a $47-million project that began in 2021 and was due to be completed in June 2026, but came to an abrupt end when, after the aid freeze in January, the U.S. State Department announced in March that it would be stopping all but a small percentage of projects funded by the U.S. Agency for International Development (USAID).
According to data provided to the International Aid Transparency Initiative (IATI), Stawisha Pwani was delivered by LVCT Health, a Kenyan nonprofit that implements health programs, in partnership with local governments. Its mobile clinics, doorstep care for mothers in remote areas, and life-saving medicines have transformed access to health services in the coastal counties of Kwale, Mombasa, Kilifi and Taita Taveta in southeast Kenya.
“The program has truly transformed lives in this village,” she says as she gently rocks her baby. “I only wish it could continue – for the mothers who still need this support, for the babies yet to be born.”
$9.2 million of the original project budget is left unspent.

Painting a picture of dependency
To get a sense of the global impact of the aid freeze, The Fuller Project analyzed data submitted by donor countries to the Organisation for Economic Cooperation and Development (OECD) and focused on four key sectors that disproportionately affect women: reproductive health, including pre- and postnatal care, delivery, infertility treatment and post-abortion care; family planning, including the provision of contraceptives, counseling and education; ending violence against women and girls; and supporting women’s rights organizations, movements and institutions. Reporters then combed through IATI data to identify specific programs, like Stawisha Pwani.
The data revealed that, while the U.S. has long been the largest donor of foreign assistance – contributing just over one-fifth of the world’s aid in 2023 – its commitment varies by sector and region.
The U.S. contributed more than half – 54% – of the foreign assistance provided by all countries for family planning and 45% of the total for reproductive health care in 2023, the last year for which figures are available, according to a Fuller Project analysis. In the same year, 26 countries received more than half of their family-planning aid from the U.S. – 19 of them are in Africa.
Kenya itself received approximately 27% of all its aid from the U.S., including more than 60% of its family planning and reproductive health care funding. Since the aid freeze, local health officials have been scrambling to continue to offer what services they can.
“As part of our immediate plans, we have requested approvals [from the local assembly] to absorb half of [approximately] 122 members of staff from the Stawisha Pwani project onto our payroll to ensure project continuity,” says Peter Mwarogo, health executive in Kilifi, one of the counties where Stawisha Pwani was implemented.
Against the backdrop of calls for Africa to seize this opportunity to rethink its reliance on aid, the Government of Kenya says it needs $522.16 million to sustain primary healthcare, procure essential medicines, and cover the funding gap left by USAID’s withdrawal. The Treasury is set to present its 2026 budget in April.
“We are reviewing current budget allocations to ensure that essential services in health, education, governance, and food security remain a priority,” Treasury Minister, John Mbadi, told parliament in March.
In the meantime, global health experts warn about the damage the stop-work order will cause, both to individuals and to health systems.
“Unfortunately, the fallout from these funding cuts will hit women the hardest, as they make up the majority of primary healthcare consumers, not just in Kenya, but across Africa,” says Dr. Stellah Bosire, executive director of the Africa Center for Health Systems and Gender Justice.
“Funding cuts don’t just disrupt reproductive health; they unravel entire healthcare systems,” Bosire adds. “These policy shifts widen funding gaps, putting millions at risk of losing access to essential healthcare services and jeopardizing vital work that has taken years to build.”
Her words are echoed by Evelyne Opondo, Africa Director at the International Centre for Research on Women.
“The progress we’ve fought so hard for is now at risk,” Opondo says. “Urgent action is needed to safeguard the lives of women and children, who will be the hardest hit by the ripple effects of USAID funding cuts.”

Back in Vyongwani, Musa Omar Mlamba, one of only two male ‘community health promoters’ at Vyongwani Health Centre, is deep in preparation for the next bi-monthly training with his group of 15 women.
“This session will focus on child nutrition, best breastfeeding practices, and maternal health. I’ll emphasize the importance of eating five balanced meals a day to ensure enough milk production,” he explains.
In a field dominated by women, he stands out – not just for his gender but for the trust and connection he has built with the mothers he serves.
“Empathy is everything in this job. My support group is thriving [because] I listen and I show up for them when they need me,” he says with pride.
But uncertain times lie ahead. For now, Mlamba has been able to continue working because he was on Kwale County’s payroll before the Stawisha Pwani program began. He hopes the county will still provide monthly stipends as before, but with Kenya’s health care system likely to be hardest hit by USAID cuts, as reported in February, it’s impossible to say how secure his employment is.
“No one has told us whether we’ll be retained or if we’ll even be paid,” he says. “With my children in school, I genuinely don’t know what to do. Who will support those who have dedicated themselves to supporting others?”
Methodology:
Data analysis for this story relied on two primary sources of information on U.S. and international aid spending: the The Organisation for Economic Co-operation and Development’s Creditor Reporting System database and data published by donors to the International Aid Transparency Initiative (IATI).
OECD data (accessible via the OECD’s Data Explorer) was used to put in context the U.S. contribution to total aid and for sectors that disproportionately affect women and girls. This data was extracted in constant (inflation-adjusted) prices to be able to look at aid over time.
IATI project-level data (accessible via the d-portal.org website) was used to identify specific projects, within these sectors, likely to be affected by the U.S. aid freeze.
Credits:
Data journalist: Claire Provost
Reporters: Allan Olingo and Jodi Enda
Data visualization: Claire Provost and Erica Hensley
Editors: Eliza Anyangwe and Maher Sattar
Additional data researchers: Allan Olingo, Louise Donovan and Erica Hensley
Photographer: Kevin Odit
Editor’s note: the story was edited to clarify that 83% of USAID projects were cancelled in March.
In April last year, classrooms at the Asa Primary School in eastern Kenya fell silent as the worst drought to hit the region in four decades forced children to stay home. When the October rains came, the lively chatter of children was restored, but with a marked difference – this time, there were hardly any girls.
When the drought was at its worst, “everyone was in survival mode,” said Roba Racha, a local government official. “The devastation caused by the drought in the area forced many children to leave school.”
After the worst was over, the boys began to return. But many of the girls never came back, said Racha, whose district southeast of Nairobi, near the Somali border, is home to pastoralist communities that depend on grazing for their livelihoods.
“You could walk into the classroom and find only boys,” Racha said. As the drought took its toll, school numbers more than halved. One head teacher in the area said his school had classes without a single girl.
It is a story repeated in many parts of Kenya, with girls much more likely than boys to have to drop out of school to help struggling parents when natural disasters like droughts or floods hit. And the changing climate is making those a more frequent occurrence.
In recent years, Kenya has been hit first by severe drought that left millions hungry and destroyed the livelihoods of pastoralist communities, then by large-scale flooding that displaced many thousands and washed crops away.
Experts in the region say girls’ education is often the first thing families sacrifice when faced with the effects of climate change. In a drought, some girls take on the back-breaking task of fetching water over ever-longer distances, while others take care of things at home as their parents seek grazing for their herds. Some are married off as children to bring income in the form of a dowry and reduce the number of mouths the family has to feed.
Their marriage potential makes girls a sort of “life insurance” for pastoralist families that have lost their livestock to drought or floods, said Jedidah Lemaron, who runs a foundation that supports girls in southern Kenya’s arid Kajiado region, home to the Maasai pastoralist community.
“The education of sons is given priority over that of daughters,” she added, with girls more likely to take on the burden of household work during periods of additional stress following a drought or a flood.
Kajiado resident Susan Nakimoru was married in 2022 aged 16 after her father lost his animals to drought. Her parents told her that if she got married, she would save her family and allow her brothers the opportunity to do the same – without animals to give away as dowry to a bride’s family they would be unable to wed.
“I was not ready to get married, but my father insisted,” said Nakimoru, fiddling nervously with the traditional Maasai yellow shawl she wore draped over her shoulder.

Research published last year by the Education Development Trust in six pastoralist regions in Kenya prone to both drought and flooding found that climate shocks typically result in increased responsibilities for girls compared to boys, leaving most out of class. The research, based on interviews with local school principals and community members, found that with each cycle of climate shocks girls were more likely to miss school and lose learning time.
It’s not just a Kenya problem. Climate-related events prevented at least four million girls in low- and lower-middle-income countries from completing their education in 2021, according to a report from the Malala Fund, an education advocacy group. If current trends continue, by 2025 climate change will contribute to at least 12.5 million girls being prevented from completing their education each year, it said.
In 2022, 15 million children in the Horn of Africa were out of school because of the drought and another 3.3 million children were at risk of dropping out, according to UNICEF estimates.
Angela Nguku, executive director of White Ribbon Alliance Kenya, a local NGO that advocates for girls’ rights warned that the substitution of unpaid care work for education is hurting the future of these girls.
“In both extremes of climate change, girls are pulled out of school to take on the role of caregivers at home. It is a never-ending cycle at the expense of their education,” she said.
Research published in 2020 by another non-profit, the International Center for Research on Women (ICRW), found that giving families cash or other support in the form of uniforms or school supplies as long as their girls attended school boosted educational outcomes.
Meanwhile, Kenya’s education ministry is building more boarding facilities in drought-prone areas to allow children to stay in school when their parents have to move to feed their livestock.
The culture around girls’ education, however, may be harder to build.
Last year Mary Enkaroi, 16, had to drop out of her school in Kajiado to help look after her younger siblings when her father left the family to seek grazing for their animals further afield. She never went back.
“There was no rain in our community. We had to walk more than five hours every day to fetch water while my father went to Tanzania to find pasture for the animals,” she said as she walked home carrying a 20-litre bucket filled with water, taking its heavy weight on her head.
“In school, I loved science and wanted to be a nurse, but I now don’t know what my future will be.”
A contractor at the centre of a BBC investigative report exposing the sexual exploitation of women working on tea plantations in Kericho, Kenya, has been allowed to contest in an election for a key tea agency, causing an uproar among Kenyan women leaders, rights activists, and international tea lobby groups.
John Chebochok, who was sacked by James Finlays Kenya (now Browns) in February 2023, is contesting for election on June 28, as a regional director of the Kenya Tea Development Agency (KTDA). KTDA is a private entity with over 600 smallholder farms in 16 tea-growing counties in Kenya.
Chebochok and other managers were filmed by the BBC’s Africa Eye and Panorama programmes in February last year, exploiting female workers in exchange for contract extensions and better working conditions. The programme included detailed testimonies of sexual exploitation by workers, as well as undercover footage implicating Chebochok as a key perpetrator.
After the programme aired, Finlays said it had fired Chebochok and others and banned them from its tea estates. It also reported the suspects to the police for investigation, but so far, no prosecutions have taken place.
Now pressure groups, led by Kenya women parliamentarians, have come out to protest against Chebochok’s candidacy, saying that allowing him to contest in the KTDA director elections is an injustice to his victims.
“We are expressing grave concerns about Chebochok’s candidacy,” said Leah Sankaire, chair of the Kenya Women Parliamentarians Association.
Given the nature of the allegations against him, she said it was imperative that his suitability be scrutinised.
“Electing him to this position will pose a risk to his juniors, especially women workers, who may be vulnerable to further exploitation under his leadership,” she said.
The Coalition Against Sexual Violence (CASV), a lobby group of 13 human rights organisations in Kenya jointly said Chebochok’s candidacy was “a grave injustice to the courageous survivors of sexual violence who have come forward to hold him to account.”
The potential election of this individual, the group said, poses a reputational risk to Kenya’s tea sector.
“We have already seen managers dismissed for similar offences rehired by other tea companies, perpetuating a culture of impunity and discouraging victims from speaking out about their abuses,” they said.
UK-based Ethical Trading Initiative (ETI), a leading alliance of trade unions, NGOs and companies working together to promote human rights in global supply chains, also condemned his candidacy and called for Chebochok’s removal from the election process.
“His candidacy undermines the work of concerned stakeholders across the Kenyan tea industry to address the endemic sexual exploitation and gender-based violence that too many workers face,” ETI said in a statement.
Ethical Tea Partnership (ETP), another UK-headquartered tea lobby group said it had written to Kenya’s electoral body, the KTDA, and the Tea Board of Kenya to express its concerns about Chebochok’s candidacy.
“We call for swift and clear action to ensure that apparent perpetrators of sexual exploitation, abuse and harassment are not employed in positions where they can continue to facilitate physical and economic exploitation and abuse,” the lobby group said.
Kenya’s electoral body, the Independent Electoral and Boundaries Commission (IEBC), is expected to hold elections for directors of the 54 smallholder tea estates managed by the KTDA.
According to KTDA, eligible candidates for the directorship must, among other requirements, have an Ethics and Anti-Corruption Commission (EACC) clearance and a valid police clearance certificate.
The police clearance certificate is issued by the Directorate of Criminal Investigation (DCI) to those who have no pending criminal investigations or convictions. The EACC certificate is also issued to those who do not have any questionable ethical and/or corruption background.
Women in East African countries are facing new tax measures that will affect their daily lives as their parliaments debate and approve budgets for 2024.
From new taxes on sanitary pads, diapers, second-hand clothes and fuel, finance ministries in Kenya, Uganda and Tanzania have proposed new tax measures that will affect the basic cost of goods and services, some of which will hit women hard.
In Kenya, women received temporary reprieve in the amended Finance Bill after parliament removed proposed additional taxes on locally manufactured sanitary pads and diapers. However, for the kenyan women, they will still have to bear with higher costs for imported sanitary pads and diapers, that is majority used by the women given production constraints of the locally manufactured one
This comes even as Tanzania increased taxes on diapers and on second-hand clothes (mitumba), a trade dominated by women.
The changes to Kenya’s Finance Bill came after weeks of pressure from activists and citizens on online platforms calling out the government’s proposals for these taxes, which they argued would push more girls and women out of the affordability of sanitary pads.
“The bill proposes a new eco-tax on sanitary pads, making them even more expensive for millions of women and girls. This move is particularly insensitive given that many already struggle to access affordable menstrual hygiene products,” reads part of a petition against the bill on change.org.
On Tuesday, in a partial victory for women, the Finance Committee of Kenya’s National Assembly bowed to pressure from various stakeholders and dropped a number of controversial clauses in the Finance Bill 2024, including the eco-tax on sanitary pads and nappies.
Kimani Kuria, the committee chairperson, said locally manufactured products will not be subject to the eco-tax as it will only apply to imported finished products.
“Consequently, locally manufactured products including sanitary towels, diapers and others that we had highlighted will not attract the eco-tax. The eco levy will only be chargeable to imported finished products,” Kimani said.
The controversial proposal had sparked an outcry, particularly from women’s groups and activists, who called on the state to address period poverty.
But nominated Senator Gloria Orwoba and period shaming campaigner pushed back against the pressure, pointing out that Parliament was not trying to impose any form of tax on sanitary towels.
“In fact, even the eco-tax that will be imposed on manufacturers will not affect local manufacturers of sanitary towels and nappies,” says Ms Orwoba.
On the contrary, Ms Orwoba says, the Finance Bill proposes to remove a policy that prevents manufacturers of zero-rated products, including sanitary towels, from charging VAT.
Kigumo legislator Joseph Munyoro had condemned the move to charge a levy on diapers saying it would burden women and mostly young mothers.
“What do young mothers do now that you want to impose a levy on diapers? Are you asking them to go back to using napkins?” Munyoro posed.
Tanzania has also proposed to increase the duty on baby diapers from the current 25 percent to 35 percent to encourage local production of the products. It has also reduced the 25 percent tax on raw materials used in the local production of these diapers.
It has also proposed to zero-rate fabrics and garments made from locally grown cotton. It has also reduced taxes on vitenge from 50 percent to 15 percent.
On second-hand clothes, Tanzania is now proposing a 35 percent tax on second-hand clothes, shoes and items. It previously charged 35 percent or $0.4 per kilo, whichever was higher. But it has siince done away with the per kilogramme limit, meaning traders will pay more depending on the volumes they bring in.
It now joins Uganda, which in January increased rates by 3 US cents per kilo from $1.16 to $1.19.
But the commissioner of customs at the Uganda Revenue Authority says they had considered changing the rates earlier in the year, but shelved the idea. We usually review the rates at the beginning of the year but we have shelved the proposal.
However, the Uganda Dealers in Used Clothing and Shoes Association says the new tax change is in place and has already forced some traders out of business.
“We are seeing most of our members dropping out,” said Lydia Ndagire, the association’s vice chairperson.
Kenya has also proposed to further increase the road maintenance levy on petroleum products from Sh18 ($0.14) to Sh25 ($0.19).
“This is expected to further increase the cost of doing business and particularly hurt informal businesses – the majority of which are run by women,” Thomas Kinyonda, an economist at Atlas said.
It has also proposed a 3 per cent export and investment promotion levy on liquid fuel (kerosene) stoves, which is expected to hit women in informal settlements and the low-income group hard.
In 2023, Kenya increased VAT on petroleum from 8 per cent to 16 per cent, which the Kenya Gender Budget Network (KGBN), the National Taxpayers Association and the Collaborative Centre for Gender and Development (CCGD) jointly said “has the greatest negative impact on marginal small and micro enterprises (SMEs) – mostly informal businesses where women are in the majority”.
The 2024 Finance Bill also proposed to increase the excise duty on mobile money transfers to 20 percent. In 2023, this had been increased to 15 percent from 12 percent. At the time, women’s groups said this was likely to create a barrier to accessing financial services, particularly for women SMEs that rely heavily on mobile money services.
However, treasury CS Njuguna Ndung’u dropped the proposed increase and maintained the current 15 percent.
In Uganda, the Ministry of Finance had also proposed in April, through the Excise Duty Amendment Bill, 2024, to increase taxes on its petroleum products to Ush1,550 ($0.42) per litre of petrol and diesel, and a further Ush550 ($0.15) per litre of kerosene, a product largely used by women in the poor and low-income bracket, from Ush200 ($0.05). However, this proposal was dropped by parliament after public outcry.
However, after weeks of protests, Kenya’s President William Ruto said on Wednesday that he would not assent to the new tax proposal and sent the Finance Bill back to parliament. However, the tax proposals remain active (not yet law) as they have already been passed by parliament. It is now expected that in the coming weeks an amendment will be presented to lawmakers to delete the entire tax bill. It will then become null and void.
It was just before Christmas. A family tradition, the first for 8-year-old Gloria Moraa. She sat holding a broken mirror in her hands, watching her aunt paint her coily hair with chemicals that would straighten every strand.
“All the young girls would get matching hairstyles for the holidays, and relaxers were fashionable back then,’’ said Moraa, who lived in Mombasa, Kenya at the time.
With each application of the relaxer, the chemicals began to irritate her scalp, and Moraa started to cry. But she said it was worth the pain when she had straight, shoulder-length hair for the first time, like the little girls on the Venus relaxer box.
“Everyone was admiring our hair, and that encouraged us to keep it relaxed,” she said.
Today, Moraa, 28, lives in Nairobi and alternates between faux locs and natural hair styles. Over the years, she said she used almost every relaxer on the market, from TCB Naturals to Dark & Lovely.
When she relaxed her hair, she had one goal: The product had to make her coily hair silky. The ingredients didn’t matter.
“I did not have the time or the expertise to discern the effects of listed ingredients,” Moraa said. “I am a consumer, not a chemist.”

She said she quit straightening her hair only recently because it seemed relaxers caused it to thin.
Growing evidence suggests the products might have far more serious consequences.
In October 2022, the U.S. National Institutes of Health found women who used hair relaxers more than four times a year were at higher risk of developing uterine cancer.
The study became a tipping point in the conversation in the United States, building on more than a decade of scientific research linking chemicals known as endocrine disruptors in hair relaxers to uterine and breast tumors. Endocrine disruptors are chemicals that interfere with hormones that regulate a range of functions such as mood, appetite, cognitive development, puberty and reproductive health.

While many Black women in the United States are rejecting chemical straighteners — and filing thousands of lawsuits against manufacturers in the wake of the study — sales of the products in some African countries continue to climb.
Tunisia, Kenya and Cameroon were among the top five countries in sales growth for perms and relaxers from 2017 to 2022, according to Euromonitor, a global market research firm. Sales in Tunisia and Kenya jumped as much as 10% over the five-year span. South Africa and Nigeria also saw growth.
“People still use hair relaxers as much as they did in the past,” said Joseph Kiemo, who runs Kiemo Hair and Beauty Studio in Nairobi.
Africa is a lucrative business market for many industries, including cosmetics. It has the youngest and fastest growing population of any continent, with an expanding middle class and a flourishing community of millionaires. With an eye on the future, companies are developing more hair and skin products to meet the needs of the continent’s primarily Black consumers.
The global hair relaxer market is expected to grow from $718 million in 2021 to $854 million annually by 2028.
The companies at the center of the U.S. lawsuits produce some of Africa’s most popular relaxers. Dark & Lovely, owned by L’Oreal, is the top relaxer in Nigeria. ORS Olive Oil No-Lye Relaxer, produced by Namaste Laboratories LLC, is in second place. In Kenya, TCB Naturals is a popular relaxer owned by Godrej Consumer Products Ltd., which describes itself as the “largest player globally in hair care for women of African descent.”
For many Black women, chemically straightening their hair is a rite of passage informed by unspoken Eurocentric definitions of beauty that favor long, straight hair and are rooted in colonialism and racism. But women also say manageability, flexibility and social acceptance drive the decision to straighten their hair.
It’s a shared experience throughout the African diaspora.
“We understand that Black women use hair relaxers for a range of reasons, some within their control, some not,” said Seyi Falodun-Liburd, co-director of Level Up, a gender justice organization in London. “And so, for us, it’s not about shaming any Black woman about making whatever choices she makes.”
Instead, it’s about government and corporate accountability, said Falodun-Liburd, who led a campaign to get L’Oreal, one of the world’s largest beauty and cosmetics companies, to remove its hair-straightening products from the market following research in 2021 linking relaxers to an increased risk of breast cancer.
Governments should do a better job of banning dangerous ingredients, she said, and they should require companies to disclose their products’ potential health effects.
In May 2022, before the National Institutes of Health study, Level Up released the findings of what it says is the first research about Black women’s experience with relaxers in the United Kingdom, surveying more than 1,000 women. The research was done in conjunction with Treasure Tress, a subscription service offering products for naturally curly and kinky hair.
Falodun-Liburd wasn’t surprised by results of one survey question asking whether respondents were aware that long-term use of some relaxers was tied to a 33% increase in breast cancer: 77% said, “No.”
“I think most Black women would not consciously decide to put something on their head that would harm them, and the issue is that most Black women don’t know [what’s in the products],” she told The Examination in an interview.
Ikamara Larasi, a campaigner with Level Up, said the study confirmed why the producers of hair care relaxers should be transparent about their ingredients.
“The price of Black women’s beauty should never be Black women’s health,” Larasi said.
‘Now it makes sense’

Mary Cunningham of New York City is among thousands of people suing the hair-care companies. Her daughter, Telichia Cunningham-Morris, died of uterine cancer more than two years ago after years of using relaxers.
When Cunningham-Morris was a little girl, she wore her relaxed hair in three pigtails that skipped past her shoulders. That was her favorite hairstyle.
Her mother started chemically straightening Cunningham-Morris and her sister’s hair when they were 6 or 7. Relaxing her daughters’ locs made managing their hair and a busy family life easier for her, Cunningham said. She typically straightened her daughters’ hair every six to eight weeks.
Kiddie Kit was the name of their first relaxer. The brand is long gone. But in an old photo from the 1980s, the relaxer box is decorated with drawings of an adolescent Black girl, her thick straight tresses sweeping her shoulders as she swims, bikes, and cartwheels with a young male admirer. Also on the box, the words Mild. Gentle. Safe.
Cunningham-Morris used relaxers for decades, then about six years ago, she and her sister made a pact to go natural, influenced by growing discussions about the harms of relaxers. But her time styling her natural hair was short-lived. On June 15, 2021, she died of uterine cancer at age 50. She spent her last days in her mother’s home in Jamaica, Queens in New York City.

Cunningham, 75, and her younger daughter, Travias Cunningham-Case, 52, believe chemicals in the relaxers caused Cunningham-Morris’s death — and their hysterectomies. Cunningham had surgery to remove fibroids nearly a decade ago; Cunningham-Case’s surgery was for endometriosis.
“It just seemed like all three of us had some kind of female problems all the time. Now, it makes sense to me that's where it came from,” said Cunningham, reflecting on the price she believes her family paid for straight hair.
Regulations lagging around the world
Some of the most concerning ingredients in hair relaxers, scientists say, are formaldehyde, a known carcinogen, and phthalates, parabens and Bisphenol A — chemicals known or suspected to be endocrine disruptors.
Bisphenol A, which appears under various names on relaxer boxes, is used to produce plastics. Phthalates make plastics more durable and parabens help preserve ingredients in cosmetics.
The Examination found that products sold in some African countries contained parabens and fragrances. Phthalates are often found in fragrances and aren’t included in the list of ingredients other than as “fragrances.”
Scientists say the cumulative effect of a combination of chemicals in hair care products, from relaxers to hair dyes, is especially concerning.
Despite more than a decade of research about the adverse health effects of chemicals in relaxers, regulation varies across Africa and the globe.
The European Union bans some endocrine disruptors in cosmetics and has proposed prohibiting the chemicals in other products, including toys. The EU says it hopes to “phase out the most harmful chemicals in consumer products” by 2030.
The United States does little to regulate cosmetics as a whole, including hair relaxers. While Brazil, Canada and other countries banned or restricted formaldehyde in relaxers years ago, the U.S. Food and Drug Administration only proposed to ban the carcinogen last fall. The agency could make a decision this month.
Some African countries, such as Nigeria, have warned consumers to avoid using hair products that contain formaldehyde.
Most countries worldwide require companies to list ingredients on product boxes. Health experts, however, say listing ingredients doesn’t mean consumers understand the potential harm of relaxers.
“The more we educate [people] about what these chemicals are and the potential adverse health effects that may be associated with them, perhaps people could make more informed decisions about whether to use these products,” said Adana Llanos, an epidemiologist and professor at Columbia University’s Mailman School of Public Health and co-author of a 2022 article suggesting policy changes to reduce exposure to potentially harmful hair products.
Llanos is working with investigators at the state-sponsored Kenya Medical Research Institute to study hair and personal care product use in Kenya.
Women in the U.S. began to sue relaxer manufacturers by the hundreds shortly after the publication of the 2022 NIH study. The lawsuits claim the companies failed to warn consumers that relaxers could increase risks of uterine and breast cancer, fibroids and endometriosis.
The companies denied wrongdoing and claimed the plaintiffs’ injuries were not caused by their products.
In November 2023, a federal judge in Chicago ruled that thousands of claims against a number of companies, including L’Oreal, Revlon, Namaste and Godrej could proceed, opening the door for a massive court battle that industry observers are comparing to the Johnson & Johnson talc-based baby powder lawsuits. More than 50,000 plaintiffs accused Johnson & Johnson of failing to inform consumers that the powder, which was heavily marketed to Black women, had been linked to risks of ovarian cancer. The company replaced the product but hasn’t settled with the plaintiffs.
Godrej, Revlon and Namaste did not respond to The Examination’s request for comments.
A L’Oreal spokesperson criticized the NIH study in an email saying it was based on “a small number of uterine cancer cases” and “does not conclude that using these products causes certain health outcomes, such as uterine cancer. Tellingly, the study states that ‘more research is warranted.’”
Additionally, the spokesperson said: “Our hair relaxer products do not contain any ingredient defined as an 'endocrine disruptor' by the World Health Organization.”
The WHO considers parabens to be “potential” endocrine disruptors. It is expected to update its definitions next year based on research from the past decade.
International advisory and regulatory bodies have long wrestled with product testing and identifying endocrine disruptors and other potentially harmful chemicals, according to scientists who study the hormone system. They note that parabens — contained in most hair relaxers — are widely considered endocrine disruptors.
Previously, Revlon told Reuters the company did not “believe the science supports a link between chemical hair straighteners or relaxers and cancer.”
Kate Akpabio, a seamstress in Lagos, Nigeria, was washing her braided hair in a salon on a hot Saturday afternoon in December. Akpabio, who has been straightening her hair with Mega Growth relaxers for seven years, had read on Facebook about the study linking frequent use of straighteners with cancer.
“It doesn’t change my attitude towards relaxing my hair,” she said. She didn’t know about the U.S. lawsuits against hair-care manufacturers.
Favour Godwin didn’t know about the lawsuits or the NIH study. Godwin, a former trader at Computer Village in Lagos, had experienced a burning and itchy scalp from some relaxers. But she said she hadn’t heard anyone talk about the health risks in Nigeria and that she didn’t plan to quit relaxing her hair.
“I can’t even cope without relaxing my hair every two months,” she said.
Opting for natural look
Even before the lawsuits against hair care manufacturers, sales of relaxers in the U.S., the most lucrative product market, were declining as a natural hair movement began to flourish nearly a decade ago.
In the United States, relaxer and perm sales declined by about 9% between 2017 and 2022.
Sales of relaxers will probably continue to dip, according to Caro Bush, a research analyst for market research firm Euromonitor. “Consumers are apprehensive of the chemical composition of these products and their impact on health,” Bush said, adding that the lawsuits intensify mistrust of relaxers in the United States.
She says the U.S. demand for natural hair care products that don't chemically alter hair texture is presenting a market opportunity.
Large companies have acquired some of the small natural hair care brands in recent years. Last year, Procter & Gamble bought Mielle Organics, a Black-owned natural hair care company. And some global companies have created products. More than two years ago, L’Oreal launched Dark & Lovely Blowout, a hair cream that says it protects natural hair from straightening with a flat iron or other heated styling tool.
In Africa, interest in natural hair products is growing alongside the sales of relaxers.
Leshme de Bruyn, who lives in Cape Town, South Africa, sells her line of natural hair care products called Miss L - Embrace My Roots.
A bad experience with hair dyes and relaxers inspired her company motto: “My products will bring you back to the natural hair you had before it started to get chemically damaged.”
De Bruyn said in an interview with The Examination, “Nowadays, they don’t do the blow dry and curls and flat irons. Younger people are saying, ‘This is the hair I’ve been born with, and I’m going to embrace it.’’’Julie Ouandji, raised in Cameroon and France, hopes to discourage African women from straightening their hair through her social media website, NappyFrancophones. Ouandji, 38, founded it to write about hair tips and inspire Black women from French-speaking countries to go natural after she quit relaxing her coily hair almost a decade ago. She had read early studies questioning the health effects of chemicals in relaxers.
Today NappyFrancophones has 218,000 followers on Instagram and 85,000 on Facebook.
“I love this name because it's like being natural and happy,” Ouandji said of the word nappy. “I want to encourage Black women to love their hair and be happy about their hair. So, that's why this name was meaningful to me.”

“I was like, ‘I’m not sure it’s going to suit me,’” she said, reflecting on how her definition of beauty was synonymous with straight, long hair. “It’s really interesting to feel that way when I think about it. It’s your natural hair. Obviously, it’s going to suit you.”
As a girl, Ouandji was influenced by the women she saw on French and American TV, none of whom had natural hair.
“I think it's really important for our generation to have more Afros in the media so our daughters and granddaughters will want to keep their natural hair,” said Ouandji, who has a three-year-old daughter.
“I would like all women to stop relaxing their hair,” she said. “But that’s utopia.”
Additional reporting by Blessing Oladunjoye from Nigeria’s BONews
The Examination is a new nonprofit newsroom that investigates global health threats. Sign up to get The Examination’s reporting in your inbox.
Sonu Bohra’s first pregnancy coincided with one of the longest dry spells she had seen in her home village, high in the Indian Himalayas. By the time she went into labor, it hadn’t rained for almost six months and the taps had run dry for days.
When her waters broke, an ambulance came to take her to the medical center in the nearest town. But they refused to admit her, saying they’d run out of water. The ambulance driver decided to take her to the next center, 55 kilometers away – a drive of several hours on the poor roads. But when they arrived, they discovered the same problem. They set off for the next health center, but it was too late – the baby was coming. In the end, Bohra gave birth by the roadside, helped by the ambulance driver.
As she watched her healthy two-year-old son playing and shrieking with joy outside their home, Bohra recalled the excruciating pain she endured giving birth to him. She knows it could all have ended very differently.

“I was terrified,” she says. “Other pregnant women have died. Everyone knows that these [maternal] deaths are high in this area. When the first hospital said no, I was worried that I might end up dying as well, like the others I’ve heard about. I started praying. My biggest concern was that the child inside me should remain alive and well.”
For nearly two decades, India has been working to transform its record on maternal health. It has expanded maternity units in rural areas, provided free ambulances to ensure women can get to them safely, and set up a vast network of community health workers known ASHA (Accredited Social Health Activist) workers to provide advice, organize antenatal check-ups and coordinate transportation to hospital when women go into labor.
The proportion of women delivering their babies in hospitals or clinics rather than at home has more than doubled, from just over 40 percent in 2005-06 to nearly 90 percent in 2019-21. India’s maternal mortality rate (MMR) has dropped from 400 deaths per 100,000 births in 2007-09 to 97 per 100,000 in 2018-2020, meeting a government target to bring it below 100 by 2020.
It’s one of the country’s biggest public health victories of recent decades and has won international praise. Yet as Bohra’s experience shows, the strategy of encouraging institutional deliveries has hit an unexpected hurdle – climate change.
India has 18 percent of the world’s population and just 4 percent of its water resources, according to the World Bank. It is the world’s largest user of groundwater, exceeding the U.S. and China combined, according to a United Nations report published in October that warned its north-western region would experience critically low groundwater availability by 2025.
As a changing climate has brought more erratic rainfall patterns that are less easy to predict than they were, water shortages have made it impossible for hospitals in drought-hit parts of the country to operate year-round. Even in major cities, some are having to delay planned surgeries during the driest times of the year – the hot months ahead of the monsoon rains, when water reserves run low. And unlike a planned surgery, labor cannot be postponed.
In 2019 the southern city of Chennai – home to about 5 million people – came close to completely running out of water, threatening essential services and forcing authorities to bring supplies in by train.

In mountainous areas like Uttarakhand – the north Indian state where Bohra lives – the problem is particularly acute because the terrain makes it challenging to build and maintain infrastructure like water pipes or truck in water by tankers, according to Parmanand Punetha, chief engineer at the Uttarakhand water department.
The main hospital in Uttarakhand’s Champawat district has struggled for years with water shortages. The main aquifer that its piped water supply comes from dried up at the height of the summer, when it has to rely on supplies coming in by truck. The hospital needs 25,000 liters of water a day, but the trucks only deliver about 10,000 a day, if they get there at all – sometimes they are blocked by landslides. A new pipeline was installed this year that draws water from a different aquifer. But with extraction outpacing the rate at which these underground sources naturally replenish, that will not last forever. “More springs are running dry with every passing year,” says Punetha.
On a hot day during this year’s dry season, a long queue of pregnant women were waiting to be seen. Rukmani Devi, 33 and six months pregnant, said she usually found the washrooms at the hospital were closed. “I really worry about giving birth here,” she confided. “There’s nowhere even to wash yourself after giving birth.”
The hospital’s Chief Medical Officer Dr KK Agarwal says he’s aware of other cases like Bohra’s, but couldn’t put a figure to it. “We have been raising this issue [water supply] with the authorities for years now,” he said. “Any project that needs government approval has to go through a long chain of paperwork for approvals… It takes time.”
With no data showing how often water-related maternity ward closures occur, it is difficult to know how many women have been impacted. But there is anecdotal evidence that it is happening elsewhere in India as overexploitation of groundwater has led the water table to drop, making it harder to source water during the summer.
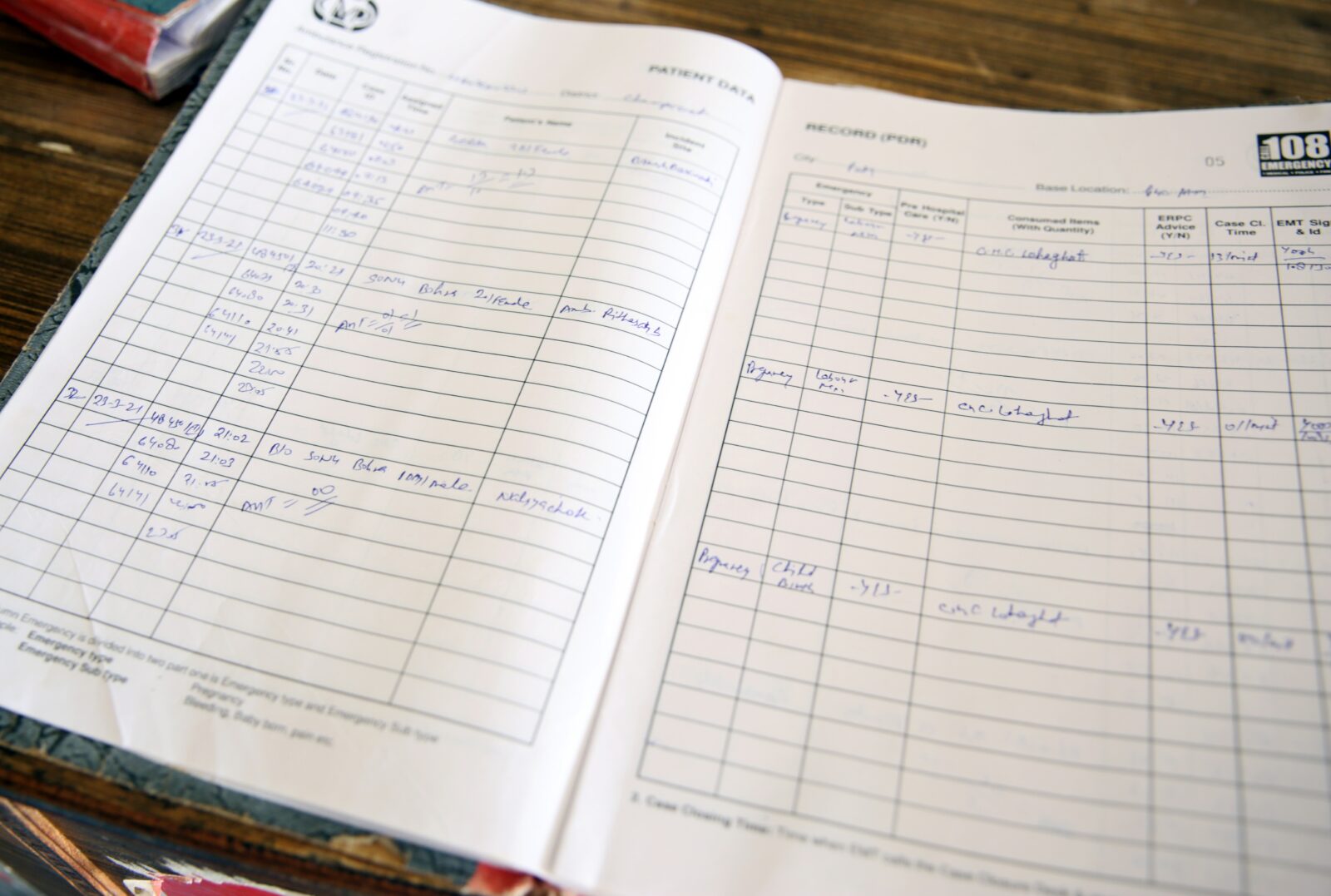
Dr Rakesh Kumar heads a small government health center in the eastern state of Bihar that relies on water deliveries by tanker during the dry season, but receives far less than it needs to operate at full capacity. The center has been forced to turn women away fearing infection if hygiene standards cannot be maintained.
“We perform a minimum of 200 deliveries a month here,” he said. “But during peak summers, the centre receives only one water tanker a day. Most days we have to ask patient’s attendants to bring water from the nearby hand pump, or are forced to send them away for delivery if we cannot manage to get water.”
In neighboring Jharkhand state, one health worker said her local primary healthcare center had suffered consistent water shortages in recent years. “The submersible pump at the health centre stopped working a few years ago as the ground water dried up,” she said. “The washrooms are never open. Women here now prefer to deliver babies at home. We have to spend a lot of time and energy convincing them to go to the nearest hospital for delivery.”
Dr. Margaret Montgomery, the World Health Organization’s lead on water, sanitation and hygiene in healthcare facilities, said closed washrooms would put women off going to health facilities. “If toilets do not work, women do not want to go to a facility; this is a real disincentive,” she said. “India has made huge gains in reversing MMR but climate change and missed indicators into national health system monitoring and unsystematic review into budgeting will compound health risks for mothers and newborns.”
Globally, 16.6 million women give birth in hospitals and clinics every year without adequate water, according to WaterAid. The international charity’s advocacy advisor for health Annie Msosa said that more than 11% of all maternal deaths and 26% of neonatal deaths can be attributed to unclean births. “Every two seconds, a woman gives birth in a facility without adequate water. Yet, there does not appear to be specific data regarding maternal health, even though the World Health Organization (WHO) resolved in 2008 to do more research on the impact of climate change on health,” she said.
Even where hospitals have adequate supplies, water shortages are impacting pregnant women’s ability to access care. Hospitals in drought-affected parts of Kenya have recorded a drop in deliveries as local nomadic or semi-nomadic communities have deviated from their traditional migration patterns in search of pasture for their livestock, taking them further away and making it harder to get to hospitals on time.
Dr. Antony Apalia, who heads the government’s health work in the worst-hit county of Turkana in northwestern Kenya, said that during the worst of the drought this year, only around one in four births there were attended by a registered nurse – well below the 70 percent recorded in October 2022.
To address the problem, authorities in arid and semi-arid areas of the country have deployed mobile health facilities using vans or even camels. They are also using chips placed in the bracelets that young women traditionally wear to track the location of new and expectant mothers and try to ensure they can access pre- and antenatal services.
In India, reducing maternal mortality remains a key policy goal, as does the impact of water shortages. But the connection between the two has received little attention, experts say. A 2019 report on water management by India’s public policy think-tank noted that at least 200,000 Indians die every year from the lack of sanitation that results from water shortages, yet its main policy focus was agriculture. Maternal healthcare was not mentioned.
“We keep hearing news reports of how a pregnant woman miscarried while carrying water home or was refused admission due to shortage of water. Yet, there is no comprehensive analysis,” says Anant Bhan, a global health researcher in bioethics and health policy.
If current trends continue, India will not meet the global target of bringing maternal mortality below 70 per 100,000 live births by 2030, warned the WHO’s Dr Montgomery.
“The problem of maternal and newborn mortality caused due to inadequate water can be solved. It’s just a matter of political will and leadership,” she said. “But if we go by the current trends, the world will fall short in ending preventable maternal mortality by more than 1 million lives.”
With additional reporting by Allan Olingo in Kenya
KERICHO, Kenya, and SAVAR, Bangladesh—Rose Nyunja was just 18 when she began working in the tea plantations of Kericho, Kenya’s biggest tea-growing region and a major source of employment for poor women in the country. For decades, she toiled away in the tea gardens, picking the leaves by hand.
Then came the harvesting machinery. Women like Nyunja started to lose their jobs by the thousands to machines that could each replace more than 100 workers.
One evening in 2020, Nyunja returned to the staff quarters to find her front door barricaded. She’d been fired. Nyunja pleaded with her supervisor to save her job — and her home. Instead, company security ejected her from the compound.
“My 26 years of service meant nothing to them,” she says, fighting back tears. “I was given one hour to remove my household items and leave. I have never experienced such humiliation and embarrassment in my life. I worked diligently for over two decades and what have I got? Nothing.”
As Kenya’s tea estates automate to improve productivity, workers like Nyunja represent a broader global trend: women are more likely than men to lose their jobs. A 2019 study from Britain found that 70 percent of jobs at high risk from automation are held by women. And this April, a University of North Carolina study found that almost 80 percent of the female workforce in the US will be affected by advances in generative artificial intelligence, compared to 58% of men.
While recent advances in generative AI have sharpened concerns about loss of jobs for white-collar workers, job losses due to companies ramping up automation have been taking place for years, as seen in Kenya. Kweilin Ellingrud, a director at McKinsey Global Institute, says her research shows that automation is fourteen times more likely to impact low-wage workers than high earners.
“I think the reason it’s grabbing headlines is because it is also affecting higher wage jobs for the first time,” says Ellingrud. “I think now generative AI is focusing and impacting jobs across the spectrum — it affects your job, it affects my job. Some of us, myself included, aren’t used to thinking: ‘How will my work have to change? How will my job change?’”
In Kericho, Roselyne Wasike, a tea picker, says her income has fallen by almost half, from $150 a month to $80 a month, as the machines take over larger shares of work on the plantation. Even those who have managed to keep their jobs cannot escape the impact of automation. Many of them are widows and single mothers.
“These machines have disadvantaged women by making them redundant instead of giving them other tasks within the tea estates,” Wasike says.
The Kenya Plantation and Agricultural Workers Union says that 30,000 women have lost their jobs as a result of automation in the past five years. About 60 percent of the 75,000 workers currently employed in the tea sector are women, down from an estimated 75 percent in 2017, according to Dickson Sang, the secretary-general of the union.
The resentment towards the machines boiled over into violence this May. Kericho residents torched nine harvesting machines worth $1.2 million in a plantation owned by Ekaterra, the producer of Lipton and TAZO teas. The clash resulted in two deaths and the arrest of Kericho’s governor. Ekaterra suspended operations for two weeks, leaving more than 16,000 employees without work.
One of the areas of dispute had been a provision in the industry’s collective bargaining agreement that workers, most of whom are women, would be kept on as machine operators. Labor leaders say multinationals have “flatly refused” to implement this.
“I do not condone the destruction of property. But these workers are now fighting back because the tea firms keep moving the goalposts,” says Sang.

Ellingrud says 85 percent of jobs impacted by generative AI will be concentrated in four job categories: food services, customer service and sales, office administration, and manufacturing. The first three are dominated by women. Even in manufacturing, women workers like Nyunja are vulnerable compared to men, who have a higher chance of being re-trained for roles involving automation.
The COVID-19 pandemic showed that women are more likely to lose jobs during periods of economic upheaval, and are slower to return to the workforce, Ellingrud says: “Women’s unemployment is more sticky.”
Her research at McKinsey has found that 12 million people will need to switch jobs by 2030, and that women are 1.5 times more likely than men to have to change their occupation. She says this means governments and businesses need to urgently take targeted actions to re-skill and up-skill women.
Automation has also radically changed the make-up of Bangladesh’s garment industry, once hailed for transforming women’s employment prospects. Women once made up over 80 percent of the garment workforce today they account for less than 60 percent. In 2019 the government projected that half a million garment workers, mostly women, would lose their jobs to automation.
At Moni Garment and Training Center in Savar, a garment hub north of the capital Dhaka, Mizanur Rahman drills his trainees on how to operate machines used for weaving and knitting. A former garment worker himself, he says being sensitive to small areas of concern goes a long way towards making women feel more comfortable.
This includes hiring female instructors for female trainees and offering flexible hours so that women can show up before or after taking care of household chores. He says the confidence women gain from their training can lead to increased recognition at work.
“Many of my trainees perform well and are promoted to supervisor or line chief positions,” Rahman says.
Supervisory roles and roles operating automated technology are likely to be among the key jobs that survive in a post-automation landscape. Both tend to be dominated by men. In Bangladesh’s garment industry, women have long made up less than 5 percent of supervisors despite being a significant majority of the workforce.
There have been some signs of success. The Gender Equality and Returns project, run by the World Bank’s International Finance Corporation and the International Labor Organization, says 60 percent of its trainees have been promoted to supervisory positions, and the number of female supervisors in the industry has jumped to 12 percent since the program began in 2016.
Abdullah Hil Rakib, a director at the Bangladesh Garment Manufacturers and Exporters Association, the country’s largest trade association for the industry, says the key obstacle to women thriving in supervisory or machine operator roles is psychological.
“It’s a barrier in our mindset,” he says. He points out that automation means less physically strenuous work for both men and women, eliminating one barrier that would have previously made some jobs less accessible for women.
“Even when a man runs a heavy automatic cutter machine, he only pushes a switch on and off. He does not need to do more,” Rakib says.
Ellingrud says about 10 percent of jobs created every year tend to be new roles that didn’t exist before, but women take up these jobs at a lower rate than men. People won’t be losing their jobs to AI, she says, but to people who know how to use AI; women who are unable to adapt risk being left out of the new economy.
Adaptation feels like a distant prospect in Kericho, where Nyunja hawks vegetables on the street to make ends meet.
“I used to be able to take care of my family and pay my children’s school fees,” Nyunja says. “Now my future looks bleak. I can barely pay my rent, let alone send my child to school.”
Maher Sattar contributed reporting from New York.
Pilot Lenaigwanai covers her mouth as she speaks. She is trying to hide her broken tooth, a bitter reminder of all she endured before finding refuge at a shelter for abuse survivors in northern Kenya.
The mother of three arrived here in July after being forced from her home by escalating violence. Her husband was abusive even before the drought that’s now ravaging Kenya’s arid north, the worst in decades. When the family’s 68 cattle — their only means of survival — died, the abuse became impossible to bear.
“He was visibly frustrated and turned the heat on me and my children,” she says. “I just think he wanted us out, because he could not provide for us anymore.”
Lenaigwanai is one of the dozens of women who have arrived at the Umoja refuge in recent months fleeing violence that they say got worse as each successive year of low rainfall plunged their families deeper into poverty. Her semi-nomadic Samburu community of pastoralists are particularly vulnerable to drought because they depend on the livestock whose emaciated corpses litter the barren lands that once provided plentiful grazing.
For these and many other women around the world, the threat of violence could become more common as climate change makes extreme weather events more intense and frequent.

Scientists have long warned that climate change disproportionately impacts the world’s poorest and most vulnerable, and negotiators from wealthy countries at the U.N. Climate Change Conference in Egypt pledged to do more to help poorer countries already grappling with its devastating effects.
Until recently, relatively little attention has been paid to its disproportionate impact on women and girls. But this year the U.N. Intergovernmental Panel on Climate Change identified a link between climate change and violence, citing the growing evidence that extreme weather events are driving domestic violence, with global implications for public health and gender equality.
A 2021 study of extreme weather events in Kenya by researchers at St. Catherine University in Minnesota found the economic stresses caused by flooding and drought or extreme heat exacerbated violence against women in their homes. The research, which used satellite and national health survey data, showed that domestic violence rose by 60 percent in areas that experienced extreme weather.
That analysis, and 40 others published this year as part of a global review in the journal The Lancet, found a rise in gender-based violence during or after extreme weather events.

Terry McGovern who heads the department of Population and Family Health at Columbia University’s Mailman School of Public Health, called the scientific evidence for this connection “overwhelming.”
“Heat waves, floods, climate-induced disasters increase sexual harassment, mental and physical abuse, femicide, reduce economic and educational opportunity and increase the risk of trafficking due to forced migration,” said McGovern, who added that the data remains limited on some fronts, including on psychological and emotional violence and attacks against minority groups.
Several academics, activists and humanitarian workers said the links between violence against women and extreme weather events need more research. Unlike the hard science of climate change, they said, the complex drivers of violence cannot easily be captured in numbers.
“The climate discourse is all about the numbers, but the evidence on violence and changes in power dynamics cannot be captured that way, and so it is not given the same weight,” says Nitya Rao, a professor of gender and development at the University of East Anglia in the U.K. “It is very difficult to make a linear connection.”

In Umoja, no one is in much doubt that the drought is driving up violence — its swelling numbers are proof enough. Jane Meriwas, whose nonprofit organization the Samburu Women Trust helps women who have fled abusive homes support themselves, says the number of women at Umoja has doubled to 51 in the last year.
“As communities and families lose their livelihoods and suffer hunger, there is increased experience of weak or broken family structures,” Most are now engaging in dangerous activities to get a meal,” she said, such as sex work and bootlegging.
With their semi-nomadic lifestyle, Samburu women are particularly vulnerable. They have little or no stable access to health facilities, police protection or support services, Meriwas said, making it harder for them to report abuse. “They are really suffering in silence.”
‘The violence peaks during the floods’
In eastern India, more frequent downpours and devastating floods are what’s driving violence. Poverty is exacerbated by sudden economic stress, and societal inequality often traps women with abusive partners or other family members because they have nowhere else to go and cannot rely on authorities for help.

A mother of five who asked to go by her middle name, Devi, to protect her identity, said she doesn’t know anything about climate change. She just knows that whenever floods come to her village in Bihar state, her husband comes home angry and violent.
With her husband working away from home much of the year as a farm hand, each season can be challenge. But the monsoon season, Devi said, is by far the toughest. That is when the rivers in her low-lying village downstream from the melting Himalayan glaciers swell to bursting, flooding large swaths of land and making farming impossible. With no prospect of work until the floods recede, her husband returns home and takes his frustration out on his family.
“The violence peaks during the floods. Everything gets worse at that time — the hunger, the stress. We have snakes coming into the house,” says Devi, 40.
“The anger gets taken out on me. There’s a lot of stress during those times and I can’t sleep because of all the tension,” she says, wiping away tears as one of her young sons leans in closer.
Devi, who shares her small thatched-roof home with her mother-in-law, has little privacy to describe the nature of the violence. But when the older woman went out of earshot, she said her husband beats her and verbally abuses her “day and night” during the floods.

Shilpi Singh, who works with women in India’s poorest state as director of a grass roots organization called Bhoomika Vihar, said she sees the connection between floods and violence as straightforward.
“It comes down to economic distress. When there is no food to eat in the house, the men vent out their frustration by beating the women, who are raised with the belief that leaving is not an option.”
For Devi, the floodwaters themselves trap her. When they surround her home, they cut her and her family off from the outside world, increasing her vulnerability even further. As she talks about her situation, she repeatedly invokes a well-known Hindi phrase that translates roughly as “I endure,” which almost always refers to women’s suffering.
“If my daughters find themselves in this situation, I will tell them, they must endure,” she said. “If there are bad days, good days must surely follow.”
Lessons from a typhoon
Scientists emphasize that extreme weather events do not cause domestic or gender-based violence, but instead exacerbate existing pressures or make it easier for perpetrators to carry out such violence.
The mass displacement that follows disasters can expose women to greater danger, according to studies in Bangladesh and parts of India.
The Philippines ranks as one of the world’s most disaster-prone countries, suffering frequent earthquakes and storms that are becoming more intense as the world warms. Nine years ago, Typhoon Haiyan — one of the strongest cyclones ever recorded — flattened entire villages in the Philippines, killing more than 6,000 people and displacing around 4 million.
When Typhoon Rai hit the Philippines in December 2021, the country was better prepared. The relatively low death toll — in the hundreds — has been attributed in part to improved early warning systems and other measures put in place by local authorities. But it caused nearly as much property damage as previous storms. Just over a year later, many victims are still living in makeshift shelters after losing their homes, and in many cases, their crops and livelihoods.

Rommel Lopez, spokesperson for the local social welfare department, said these stresses often acted as triggers for abuse within families in a country where violence against women is common. One in every four Filipina women aged 15 to 49 has experienced physical, emotional or sexual violence from a husband or partner, according to a 2017 demographic survey conducted by the Philippine Statistics Authority.
“When there’s a calamity or disaster or conflict, that can put families in difficulties. The situation at evacuation centers is a contributing factor,” Lopez said. “It makes them agitated. It adds to their frustration. When someone is frustrated, they could reach a certain point and that could trigger [violence].”
Aira Nase, 37, has been running away from violence all her life. Her mother suffered beatings from her partner and as a young girl, Nase vowed never to be like her. She was proud of raising her three children alone, taking on jobs in Manila, the capital, to provide for them.
When covid hit in 2020, she decided to leave the city and take her family back to her home province of Southern Leyte on the eastern side of the archipelago that makes up the Philippines. She got together with a local fisherman, and for a time the couple enjoyed a quiet life. They would occasionally quarrel over his drinking, particularly after Nase became pregnant in 2021, but never got into physical fights.
All that changed after Typhoon Rai made landfall shortly before Christmas 2021, devastating swaths of the country and destroying the couple’s home. They spent the holidays in a school library that doubled as an evacuation site, remaining there until May.
Her partner began drinking more frequently and the couple fought daily. Then Nase’s breast milk dried up, but the couple could not afford formula for their two-month-old baby. Her 16-year-old daughter gave birth to a premature baby who died after they could not afford hospital care.
The tensions between the couple peaked in February, when Nase’s partner returned drunk and rowdy to the library, disturbing other evacuees. Nase said she tried in vain to quiet him down. When she went to leave, he kicked her before rushing out of the room. Nase passed out and when she regained consciousness the next day, he was in jail.
“It was a very stressful time for us. We were broke and jobless. He was hotheaded and often drunk,” Nase said. “I told him: you’re not the only one who suffered from the storm, our neighbors did too. If you have a problem, why don’t you talk to me?”
There’s no official data showing how extreme weather disasters affect levels of violence against women and girls in the Philippines. One study, based on in-depth interviews with 42 people including survivors of Typhoon Haiyan, aid workers and government officials found reports of domestic violence, sexual violence and incest had increased in its aftermath. A separate survey of more than 800 households in the affected area carried out by the International Federation of the Red Cross and Red Crescent Societies (IFRC) found increases in both early marriage and domestic violence.

Humanitarian organizations working in the Dinagat Islands, which were badly hit by Typhoon Rai, sought to break this pattern. They launched a poster campaign highlighting where women can go for help if they are facing violence at home, along with a phone number to call.
For the Samburu women at Umoja, escaping the twin pressures of violence and drought has become key to their survival.
Rose Lairolkek sat in the little remaining shade afforded by the cluster of traditional mud-roofed huts that make up the refuge. She recounted how her husband came home angry after discovering all his cattle had died and attacked her, and how she still bears the scar on her right shoulder more than two years later.
“It almost cost me my life.”
Related Stories:
Lessons from Texas: Advocates Warn of Extreme Weather’s Link to Domestic Violence
DANDORA, Kenya– As Winnie Wanjira rifles through mountains of waste at the Dandora dump in Nairobi, it’s not the discarded needles that most bother her. Nor the metal scraps that could shred her skin like paper. It’s not even the hot sun that beats down on the rancid rubbish, making the 36-year-old feel so dizzy she struggles to fill her sack with plastic bottles.
Today, the mother of six is anxious about her period. It’s heavy, she says. So heavy she spent the last two days lying down in her windowless, single-bedroom home, unable to move. “The bleeding… is no joke,” she tells The Fuller Project and VICE World News. “I cannot come to work, I cannot go anywhere.”
Now, on the third day, she’s back, hoping the jumper tied around her waist will cover any stains. “And it’s, like, black, not even the normal colour of periods,” she says. “That place… It kills. It really kills.”
As far back as 2007, the United Nations Environment Program warned that Dandora posed a serious health threat to those working and living nearby. Yet while it is understood that exposure to the toxic chemicals found on dumpsites can result in cancer, respiratory problems and skin infections, scientists and environmental campaigners say relatively little attention has been paid to their impact on the reproductive health of waste pickers, who are often women. Materials such as plastic and e-waste contain a cocktail of chemicals that studies show can disturb the body’s hormone systems. As ever-higher volumes of trash continue to end up in landfills, informal workers like Wanjira will be on the front lines of what scientists are calling an emerging issue of global concern.

For years, acrid smoke has billowed across this sprawling dumpsite, which covers an area of the Kenyan capital the size of 22 football pitches. On windy days, clouds of smoke engulf the nearby neighbourhoods. “You can’t breathe,” a woman who works in a nearby pharmacy tells The Fuller Project and VICE World News.
It’s not just an issue at Dandora. Across Kenya’s dumpsites, a potentially toxic mix of everything from empty milk cartons to old tyres are being destroyed through open burning, according to a 2017 report by the government and the United Nations. Around the world, many of the estimated 20 million waste pickers in countries such as India, Ghana and Vietnam likely face similar health concerns. Estimates vary, but studies show this informal workforce is often mostly women.
“This is a global problem,” says Griffins Ochieng, executive director for the Centre for Environmental Justice and Development (CEJAD), a Nairobi-based nonprofit focusing on the problem of plastic waste. “Any dumpsite – anywhere there is plastic pollution – women will be impacted.”
This is because many materials that end up as waste contain toxic substances. Plastics and e-waste are known to contain and leach hazardous chemicals into the environment, including endocrine-disrupting chemicals (EDCs), which have been linked to reduced fertility, pregnancy loss and irregular menstrual cycles, among many other conditions. Burning them releases or generates a number of highly toxic chemicals and heavy metals, with reported similar effects. The toxins are not only in the air but also in the soil and water, and for the many waste pickers who eat from the landfills, in their food, too.
While men frequently take on more supervisory roles, women often spend the entire day rummaging, says Ochieng. “They’re in the thick of things… but the environment is a threat to their human health.”

Globally, the amount of trash we produce – and where to put it – is a growing problem. Each year, the world generates 2.01 billion tonnes of household waste, the equivalent of more than 6,000 Empire State Buildings being collectively chucked out every 12 months. By 2050, the number is set to rise by more than 70 percent. In low-income countries, over 90 percent of waste is either dumped in the open or burned.
It’s why waste pickers, like Wanjira, are often described as the backbone of waste and recycling industries. They’ve stepped in, an informal, often invisible workforce relied upon by governments in parts of Latin America and Asia and across Africa. Spending long days bent over, picking up and sorting waste discarded in streets and dumpsites, they recover more recyclable materials than formal waste management systems yet represent some of society’s most marginalised populations. In Kenya, roughly 3,000 to 5,000 waste pickers scatter across Dandora’s hills every day. Around the country, local organisations estimate the numbers reach nearly 50,000, although there is no official total.
If Wanjira’s heavy, painful period had been a one-off, she might have been a little less worried. But she’s faced the same issue – often twice a month – for roughly 20 years, she says. When Wanjira was about 13 and her family could no longer afford school fees, she dropped out and started working with her mother, Jane, who was also a waste picker. Within several years, Wanjira’s problems with her menstruation started, she says.
She’s not alone. In interviews with 32 women across Dandora and Gioto, another vast dumpsite in Nakuru, a three-hour drive from Nairobi, 21 women said their periods are irregular. Many, like Wanjira, face very heavy, painful periods once or twice a month. Others wait eight months for theirs. One in three say they have suffered serious issues when pregnant, including miscarriage, stillbirth and premature birth. About 10 to 15 percent of pregnancies worldwide end in miscarriage, according to March of Dimes, an organisation that works on pregnancy and postpartum health, while stillbirth and premature birth are much rarer.

One 59-year-old woman who has worked at Dandora for nearly three decades is being treated for uterine cancer.
“We hear these issues all the time,” says Joyce Wangari, a 23-year-old waste picker who has worked at Dandora since she was 12. She only gets her periods every two to three months. “It’s so common.”
There’s no definitive proof that the problems experienced by these waste pickers are caused by exposure to toxic chemicals, but it’s highly likely to be an underlying factor, according to Sara Brosché, science adviser at the International Pollutants Elimination Network (IPEN), a global network dedicated to eliminating toxic chemicals.
“The evidence is strong,” she says. “But the connection between toxic chemicals and impacts on women hasn’t really been talked about that much. It’s such an important but overlooked issue.”
In WhatsApp messages, Daniel Wainaina, chief officer for public health at Nakuru County, says waste pickers’ health is not individually analysed but that it would be “an interesting area for prospective studies.” He did not answer specific questions about the impact of toxic chemicals on reproductive health.
Neither the Nairobi county government nor the national governing body that oversees environmental policies replied to multiple requests for comment.
Doctors in several medical clinics near the dumpsites point out the workers’ choice of family planning likely plays a significant role. Many birth control options, including the pill, implants and intrauterine devices (IUD), can produce menstrual cycle changes. Genetics, nutrition and poor living and working conditions may also play a part. Most waste pickers handle trash without gloves or masks, and they often live near or on the dumpsites, which intensifies their exposure to health risks.
Yet one-third of those interviewed say a medical professional informed them their reproductive health issues either were or could be connected to their working environment. Some started picking trash as adults, and say they had no reproductive issues before then. Others say they aren’t using any contraception, or their problems persisted after they stopped taking the pill or removed the implant. Several say they started taking hormonal contraception with hopes of regulating their menstruation – often with little success.
“Before I came here, my periods were normal,” says one waste picker, whose name we are withholding due to safety concerns. “But then it came heavy, and so many times in a month.” She began picking trash when she was roughly 30 years old. Now 58, she is no longer menstruating, likely due to menopause. “But that smoke enters your body. You feel weak, so weak.
“Also the things that we’re sitting on,” she continues, pointing to the brightly-coloured bags filled with shreds of plastic film piled up beneath us. “They have chemicals in them. You never know if they affect you, but eventually you start feeling pain. In my chest, mainly, and around my abdomen and back. When I sit down, I feel like something very sharp is piercing me.”

Considered virtually worthless 20 years ago, plastic is now in high demand. Wanjira can sell a 1kg bag of plastic bottles to middlemen or traders for the equivalent of 13 cents (cotton, by comparison, sells for 2 cents). On a good day, she earns roughly $2.50; on a bad one, just 80 cents. As demand for packaged, mass-produced products has grown, plastic production has exploded, overwhelming the world’s ability to deal with it. Only 9 percent is successfully recycled, with the bulk ending up in landfill, incinerated or leaking into the environment, according to a report by the Organization for Economic Cooperation and Development. Unless action is taken to limit its use, plastic production and disposal are projected to triple by 2060.
“It’s completely out of control,” says Ochieng.
As plastics degrade into microplastics or are burned, people who live near dumping sites or the surrounding environment face health risks from toxic chemicals. These can include dioxins, mercury and polychlorinated biphenyls, or PCBs, which were banned in the US in 1979 and have been labelled probable carcinogens.
Yet studies indicate just how easily those chemicals can find their way into our food. At the world’s largest e-waste scrap yard, in Ghana, the unusable wires and spare plastic bits from old electronics are set alight. The eggs of chickens that foraged nearby contained the second-highest level of brominated dioxins ever measured, according to a 2019 report by IPEN. The chemicals can harm developing foetuses, interfere with hormones, and cause reproductive problems and cancer.

“Come,” says Wanjira, leading the way across a makeshift wooden bridge towards her home. The water in the river below is a murky grey, old plastic containers littering the banks. Inside, Wanjira’s mother, Jane, sits quietly threading small orange beads onto string. She now sells bracelets to earn money, having quit working at Dandora several years ago.
“I was constantly getting sick,” she says of her 40 years picking waste. Jane first started in the early 80s, several years before Wanjira was born. While her periods were never impacted, she says, she now suffers from diabetes, arthritis and high blood pressure.
Jane’s now in her early 50s, and it’s possible her health issues are age-related, says Pauliina Damdimopoulou, a senior researcher in chemicals and female fertility at the Karolinska Institutet, a medical university in Sweden.
“Maybe she would have gotten sick anyway,” says Damdimopoulou. “But it does sound like the environment is so toxic that most health issues could be attributed to it. How the toxicity manifests in individual cases is very hard to say.”
Related: Air pollution’s impact on women’s health is slipping under the radar, public health experts warn
For second-generation waste pickers like Wanjira, the health risks are greater, adds Damdimopoulou. As chemicals in the body of a pregnant or lactating person may transfer to a foetus or infant via the placenta or through breast milk, it’s possible they were exposed before they were even born, she says. And they could pass those chemicals on to their children. When exposure takes place early in life, either in the womb or during childhood, the health impacts can be worse because the body is still developing.
“And the longer you’re exposed to many of these chemicals, the higher the levels,” says Damdimopoulou. “My prediction would be that these women would be even more affected than the others.”
Twelve years ago, when Wanjira was pregnant with twins, she switched from picking trash deep in the dumpsite for a quieter job collecting plastic bottle tops along the edges. She felt a pressure in what she describes as her private parts, but tests from the hospital showed no issues, she says. After previously losing two pregnancies – one through miscarriage, the other a stillbirth – she decided to take it easy. Doctors had already told her toxins from the dumpsite were impacting her menstrual cycle, and she wanted to protect herself.
The twins arrived safely, but they have asthma. Another child has epilepsy, she says. She can’t afford the regular 4,800 Kenyan shillings ($41) for their inhalers, instead using those she finds discarded on the dumpsite. “I don’t look at the expiry date, which I know is risky.”
She remembers a doctor suggesting the twins were impacted in her uterus by the toxins she inhaled at the dumpsite. “But there is nothing I can do,” she says. “My kids must eat.”
Rita Mokhwana, a nurse in a nearby clinic in Dandora, said she wasn’t surprised by the problems the waste pickers faced. She estimates about half her patients work on the dumpsite. Miscarriages are a daily routine, and she treats three to four people a week with menstruation issues. The majority are not on birth control. “Mostly the cause is the dumpsite – the smoke, pregnant women overworking themselves,” she says.
Many waste pickers are reluctant to voice their concerns out of fear the county government could close the dumpsite. Most know the environment is not good for their health, but it’s their livelihood and a vital, if treacherous, lifeline. Since the Dandora site was declared full in 2001, there have been multiple efforts to clear the area — the latest in July last year, when a court ordered the county government to relocate the landfill to a more environmentally friendly site where waste is properly separated and recycled within six months. Yet the dump is still in operation. Every day, another 850 tonnes of waste from the city’s 4.3 million residents enters its overflowing walls.
As the leaders of the newly formed Nairobi Recyclable Waste Association, Wanjira and Wangari are organising on behalf of roughly 300 members to promote and protect the rights of waste pickers. Both women are currently hustling to recruit new members. The larger the group, the more their legitimacy and bargaining power grows when calling on the government for safe and healthy working conditions, says Ochieng of CEJAD.
“We don’t fear to take a stand because we represent the waste pickers,” says Wanjira. “If the government tries to kick us out, we can run to court and say we have rights, we work here, where do you want us to go?”

If the waste pickers in Kenya want to demand change, they’ve timed it well, says Ochieng. Two months ago, world leaders met in Nairobi and agreed to develop the first-ever global treaty that would restrict the growth of plastic pollution. The aim is to not only improve recycling methods and tackle the world’s plastic waste problem but also put curbs on plastic production.
The details will be hammered out over the next two years, but Ochieng is hopeful. For the first time, the new agreement formally recognised the significant contribution of waste pickers in the plastics economy. While it’s not yet clear how much will change, a new waste management bill in Kenya pushing for households to segregate their trash also represents a shift in thinking – one where reusing, repurposing or recycling materials is prioritised over simply throwing away.
“And the waste pickers need to be part of these formal conversations,” says Ochieng. “That’s the idea around their organising… Someone has to fight for their role.” Back at Dandora dump, Wanjira is flicking through a pile of crumpled papers ripped out from a textbook. On each side, a list of women’s names runs from top to bottom – her latest recruits to the waste picker association from a nearby dumpsite. “I signed up 70 mamas the other day,” she says, smiling. She is nervous, though. She thinks the government will chase her away if she complains about the air pollution.
“But I am not the only one. Women on the dumpsite are suffering. They need our help… their stories need to be heard.”
Additional reporting by Eriss Khajira
Maureen Faustina, 29, works as an operations officer in Nairobi, but recently moved out of the city to save on rent. This is her story in her words, edited for length.
***
I used to live at Fedha Estate in Nairobi’s metropolitan area. I now live in a sleepy little town along Kangundo Road, about 40 kilometres (25 miles) from the capital city. I have to wake up very early to get to work on time.
My husband and I drive our family car from our homestead to a nearby gas station and park it there. We then board a matatu (public minibus) to work, to cut back on fuel costs. We would normally drive all the way to work, but the fuel prices are too prohibitive. A thousand Kenyan shillings’ ($9) worth of fuel could last an entire week, but recently that amount barely lasts a day.
A lot of things have changed since the big move. None of these changes are out of my own accord, but I have been caught between a rock and a hard place. In this economic climate, something had to give. We had to move houses to cut costs on rent. I no longer spend my evenings cooking and doing homework with my three children. The time I spend commuting is so long that by the time I get home, my children are already asleep.
Since the introduction of a four-term academic year, we have had to live frugally in order to raise school fees. My husband asked me the other day why we were not having meat for supper. Well, I have had to make major changes to our diet because of the skyrocketing food prices. I buy more vegetables and plant-based proteins than meat and milk products.
I would love to buy some meat but I cannot buy a kilogram for 520 shillings when the same used to retail for 300 shillings.This is part of the reason we moved to the outskirts of Nairobi.
There is a sense of community where I live. It is easy to barter commodities with my neighbors in case I run out of something. I started growing maize in my backyard that I exchange for vegetables. I also get cow milk from my neighbors since it is cheaper than pasteurized milk from the supermarket.
I hope my children do not feel the pinch of these dire times. We moved them to different schools where they provide for a book fund. My two eldest children can get books from their schools and I don’t have to constantly buy them at the beginning of every academic year.
I no longer buy their school shoes from Bata because of the hefty prices. School shoes used to retail at 1,500 shillings but today the same pair goes for 4,000. There are more affordable local shoemakers in Limuru town where I have started purchasing shoes from.
I am contemplating taking my youngest child who is two years old to school early. Even though the requisite age for starting is four years, it would be cheaper for him to be in school than keeping our live-in nanny.
Sometimes I forget about my personal needs. I don’t remember the last time I went to a spa. I am not complaining, but I miss having time and money for myself. Part of the reason why I cut my dreadlocks was to reduce the amount of money I spend on hair maintenance.
I have to do everything within my capability to ensure my family is well taken care of. I do not regret the sacrifices I have made because I know I am not in this alone. I talk to my colleagues, relatives and friends and the situation is the same across the board. In the meantime, I am taking one day at a time.
Editor’s note: The Fuller Project and the Nation produced this dispatch as part of our “Financial Pandemic” project, a collection of firsthand accounts on how the cost-of-living crisis is affecting the daily lives of women around the world.


Financial Pandemic: ‘Sri Lanka is not a country for poor people now’

Financial Pandemic: A Lima woman is fighting to feed her community as food prices soar
Feroza Hussein, 58, lives on the outskirts of the capital Colombo with her husband, a day laborer who has struggled to find consistent work since the start of the pandemic. She recently had to quit working because of her high blood pressure, and they have been hit hard by rising costs. Her comments have been translated from Sinhalese and edited for length.
***
The price of gas had been increasing over the years and by last year we were struggling. But in 2022 the prices have exploded. A cylinder of 28 pounds of gas went from US$4 (1,493 Sri Lankan Rupees) to $7.43 and then to $13.50 within a few months.
Given that our monthly income is about $50 to $55, you can understand that cooking with gas is no longer possible. So I sold the cooker as well as the gas cylinder and switched to kerosene. Not only poor people like us who make a living through day labor, but people who were doing government and private sector jobs also started using kerosene.
In the last year, I went from using LP [liquefied petroleum] gas for cooking to kerosene, and now firewood. I live in a single room with my husband, and cooking with kerosene and now firewood is a risky business. Not that cooking with gas in a small room is not without risk, but with kerosene and firewood the risk of something catching on fire increases. But for poor people like us, there is no choice.
So, I had to be careful with the kerosene cooker. I have also heard of stories that the fumes from kerosene cookers can make you lose consciousness, so I always kept doors and windows open when I cooked using the kerosene cooker.
But kerosene was cheap. At a gas station I could buy 0.2 gallons of kerosene at $0.24. Because my husband and I eat only twice a day and we cook little, we could make do with 0.66 to 0.88 gallons of kerosene a month. This was a great relief for us.
But at the beginning of the year, it became harder to purchase kerosene at gas stations. People had to wait for 10-12 hours in queues to buy kerosene. I have high blood pressure and can’t wait. If my husband goes and waits in line, he won’t be able to work, and we will have to starve.
So, we started buying from the black market. There were vendors that sold a bottle at $0.28 initially and then they increased the price to $0.42 a bottle. But by April there was no kerosene at all.

Then we decided to switch to firewood, I mean what else can we do. Not only is this more dangerous than the kerosene cooker but it also takes more time and I need to be next to it throughout the cooking process. The smoke is a nightmare for people like us who live in one small room. Our bed and clothes are next to the stove, so I must worry about that too.
Sri Lanka is not a country for poor people now. The price of food is through the roof. The cost of a two-pound bag of rice is at least $0.58 now, which is twice what it used to be in January.
We used to make roti but we have stopped that after flour prices went up. My husband loves bread, but a loaf of bread is now about $0.42. My husband also tries to find free vegetables and leaves that are edible, on his way home after work.
Even the price of milk powder is unbearably high. A small packet of 0.15 pounds is now $0.42, but we try to buy it because we are used to having a milk tea or a coffee in the morning. That’s the only luxury we have.
I go to a government clinic once a month. There is also a shortage of medicine in the country, but so far, I am getting my medicine free of charge from the government. If that stops, I will just have to stop taking medicine and prepare to die.
***
Note: A US dollar was trading at 380 Sri Lankan rupees on May 12, 2022
Editor’s note: The Fuller Project and the Nation produced this dispatch as part of our “Financial Pandemic” project, a collection of firsthand accounts on how the cost-of-living crisis is affecting the daily lives of women around the world.

Financial Pandemic: For a refugee in crisis-hit Lebanon, even buying bread is a struggle

Financial Pandemic: As living costs spiral in Kenya, a mother sacrifices to spare family from ‘dire times’

Financial Pandemic: A Lima woman is fighting to feed her community as food prices soar
Asencia Tuamana, 55, is a community organizer in Cerro Papa, a neighborhood in the south of Peru’s capital, Lima. She started the Bello Horizonte olla común, or communal kitchen, in September 2020 to share resources during a nationwide lockdown that left millions of Peruvians with no income. Ingredients are bought in bulk, which keeps the price down, and meals are sold at cost, with the proceeds used to buy more ingredients. Her comments have been translated from Spanish and edited for length.
***
Nothing could have prepared me for what the last two years have been like. This was always a rough neighborhood, so it was pretty clear from the start that being a community organizer was never going to be easy, but the pandemic and current rise in prices have been more difficult than I could have anticipated. I’ve always believed, however, that we’re put on this planet for a reason, and it is not to sit still and acquiesce.
It’s funny, when we first set up the communal house, people mocked us. They said we were wasting our time, that we had nothing better to do. They even said it to my face. But our olla común serves up to 140 people every day from Monday to Friday, and a lot of the people that used to make fun of us come here for their daily lunch.

We started the olla in the first year of the pandemic. After a while people were going to bed on an empty stomach. Everything was borrowed: pots, plates, wooden spoons. I went door to door, asking if there was anything anyone could spare. We managed to raise 100 soles ($27) to buy the ingredients we needed for the first few ollas. We’ve learned a lot since, but making ends meet has become increasingly hard. All the ollas I know have raised their prices by at least 50%. We’ve managed to limit the increase to between 2 and 2.5 soles, but it takes a lot of work. The price of some vegetables has tripled, eggs have doubled. A gallon of gas used to cost 35 soles but it can now go up to almost 60 soles.At the olla we always serve an entree, usually soup, and a main course. We make sure to have carbs and some sort of protein: chicken feet, cow lungs, maybe eggs when they’re not too expensive. Due to the rise in food prices, we’ve been told by the government we can collect vegetables that are being thrown out from a nearby market after closing time, but it’s easier said than done. Sellers yell at you and insult you, and I don’t want to expose the women here to that kind of treatment. It’s humiliating and you’re too vulnerable. So far, I’ve made the decision to keep buying vegetables. I do know of a place nearby where we sometimes find decent bell peppers and other vegetables that were going to waste, so we sometimes go there to collect them and just cut out anything that’s rotting.

My proudest achievement is our vegetable patch. It has allowed us to endure the worst moments. During the farmers’ protests nothing was even being sold and, if it was, there was no way we could afford it. Our vegetable patch got us through that. I grow beets, leeks, celery, broccoli and what not. But we don’t have running water here and just doing the dishes and watering the plants is getting more expensive. I used to pay 30 soles for water and it’s now up to 70 soles.
But it’s not just the money, everything is harder now. I mostly work the vegetable patch alone. It’s difficult to think and act collectively when things are so rough, especially when you don’t have that drive ingrained in you. I’m not sure why I see things differently. We came to Lima when I was a child, after my father was murdered in times of terrorism, and I sometimes think that shaped me. I know we can’t get far on our own.
I still have big plans for our neighborhood. I’d love to expand our vegetable patch, but I need help… and money. Every week, I set some money aside for our emergency fund. I was hoping to eventually use it to set up a water pipe, but with rising prices it’s getting harder not to dip into the fund just to cover basic costs. We’ve had to get creative. We now compost everything and use it in the patch. We’ve also learned how to reuse cooking oil to make organic washing detergent. I water the vegetable patch with the water we use to rinse the pots and dishes and so on. It may not sound like a lot, but it all adds up. We always find new ways.

Editor’s note: The Fuller Project and the Nation produced this dispatch as part of our “Financial Pandemic” project, a collection of firsthand accounts on how the cost-of-living crisis is affecting the daily lives of women around the world.

Financial Pandemic: For a refugee in crisis-hit Lebanon, even buying bread is a struggle

Financial Pandemic: ‘Sri Lanka is not a country for poor people now’

Financial Pandemic: As living costs spiral in Kenya, a mother sacrifices to spare family from ‘dire times’
In late March, reports of violence against women began flooding into newspapers and onto T.V. screens as the pandemic picked up speed around the globe. With over half of the world’s population living under lockdown, millions of women were trapped with an abusive partner, cut off from extended family and often with reduced access to support services due to COVID-19 restrictions. For many women, the pandemic equalled a two-fold threat: coronavirus infections and being locked in a confined space while facing danger on a daily basis.
In the past nine months, all types of violence against women and girls, particularly domestic, have intensified, according to the United Nations (U.N). Now, despite the majority of countries around the world tackling the coronavirus head-on, many of those same nations have failed victims of abuse through inadequate planning, funding and attention.
“Men’s violence against women is also a pandemic, one that pre-dates the virus and will outlive it,” said U.N. Women Executive Director Phumzile Mlambo-Ngcuka in a statement to mark the annual International Day for the Elimination of Violence Against Women last month. “It too needs our global, coordinated response and enforceable protocols. It too affects vast populations of all ages.”
Worsening the situation is many governments’ failure to include protection for those abused as part of their COVID-19 response plans. According to data from the U.N.’s COVID-19 Gender Response Tracker, most nations are not doing enough to address the “economic and social fallout” caused by the crisis. Less than a quarter of the 206 countries analysed by the tracker treated violence against women and girls-related services as an “integral part of their national and local COVID-19 response plans,” with very few providing adequate funding for related services.
The global response has particularly failed women and girls in refugee settings and, displaced and post conflict environments, according to a new report from the International Rescue Committee. Local women’s groups were critical to maintaining essential gender-based violence support services during the pandemic, it adds.
Set against this harrowing backdrop are ongoing economic pressures and widespread job loss, which have contributed to what the U.N. are calling a ‘shadow pandemic’. In April, the agency estimated that for every three months of lockdown that continued, an additional 15 million women were expected to be affected by intimate partner violence.
Last year, some 243 million women and girls experienced sexual or physical violence from their partner around the world. In 2020, reports of domestic violence, cyberbullying, child marriages, sexual harassment and sexual violence have increased globally, added Mlambo-Ngcuka. The abuse is as global as the pandemic: from Brazil to China, Uganda to Nigeria, its alarming rise has been well-documented.
In the U.K, the British government failed to prioritise domestic abuse in its lockdown arrangements and did not provide help for abuse victims fast enough. At least 16 domestic abuse killings took place between 23 March and 12 April in the U.K, much higher than the average for the time of year, according to the Counting Dead Women project.
Around the world, distress calls to abuse hotlines sky-rocketed, though official data isn’t always clear-cut.
A women’s hotline in Uganda reported a more than five fold jump in the number of average weekly domestic violence cases reported once lockdown started in late March. The British charity Refuge, meanwhile, reported a 700% increase in calls on one single day in April. But in other places, such as Italy, official numbers decreased as women were less able to seek help through regular channels while at home with their perpetrators, say rights groups.
“Sometimes, reported abuse cases are falling dramatically and you would think that violence is going down, but it’s just the opposite,” Christina Wegs, the global advocacy director for sexual and reproductive health and rights for CARE, told the Washington Post in September. “The drop is reflecting that women and vulnerable people are not able to report what’s happening.”
In fact, evidence shows that the pandemic has resulted in significant increases in gender-based violence in nearly all countries, according to UNAIDS, especially for women trapped at home with their abusers.
Data compiled by U.N. Women in April this year across ten countries, including the United States, Singapore and Argentina, showed a heightened demand for access to women’s refuges and other support services this year, while shelters reached peak capacity in many places, made worse by the fact that some were repurposed for additional COVID-response programmes.
In the early stages of the pandemic, some countries did take steps to respond to the warnings of soaring domestic abuse rates. Canada allocated $50 million to women’s shelters and sexual assault centres, while the government in New Zealand included preparations in its lockdown plans from the beginning (and have since pledged $141 million to domestic and sexual violence services). France, Italy and Spain each set up programmes to house people in hotels if existing emergency shelters were at capacity.
In Bosnia-Herzegovina, there are also plans to support organizations running shelters, while in Colombia and Sweden financial resources are being allocated to support gender-based violence survivors.
There has also been action on the grassroots level. Women have been at the forefront of protests over the past couple of months in a bid to draw attention to domestic violence and demand government action. In July, large-scale protests erupted in Turkey over the killing of 27-year-old Pinar Gultekin, a university student whose former partner was later arrested for her murder. Gultekin is just one of 278 women killed in Turkey because of her gender since the beginning of the year, compared to at least 474 in 2019, the highest rate in a decade, according to the campaign group We Will Stop Femicide Platform. The final figures for 2020 are expected to be higher, given coronavirus lockdowns.
Meanwhile, in Ukraine last month, feminist group Femen staged a topless protest outside President Volodymyr Zelensky’s office to mark the International Day for the Elimination of Violence Against Women. And in Mexico, protests to fight physical and sexual violence have taken over the city, with feminists kicking government workers out of the Human Rights Commission building last month to use it as a makeshift shelter for women fleeing violent homes.
But many fear this could be too little, too late. “The economics of violence are simple and devastating,” says Mlambo-Ngcuka from U.N. Women. “No one gains. Everyone loses, and we have to turn this around. We know what it takes to fight a pandemic. Now we need the will to do it.”
One morning in September, Ashura Mciteka was sitting at home when her daughter burst through the door. “Come and see,” cried 10-year-old Ella, tugging her mother’s hand. Together they retraced Ella’s steps along a rocky, uneven pathway in their low-income neighbourhood in Nairobi, Kenya’s capital, to where the young girl had been playing.
The pair spotted it easily: a tangle of lifeless limbs in a muddy puddle.
As a trained health volunteer, 38-year-old Mciteka is frequently called to make home visits, treat common illnesses and arrange hospital referrals for her neighbours. She immediately knew what she was looking at: a recently aborted foetus.
“I’m also a mother, so I know,” she explains over the phone one month later, her voice low.
Over the last six months, across Dandora, an array of apartment blocks and informal settlements next to one of the largest unregulated landfill sites in Africa, Mciteka has directly dealt with or heard of at least 30 abandoned foetuses or newborn babies.

Five of these were found in the same tip minutes from her home, discovered by someone in her community – a rubbish collector, local resident and even her own young child.
In 2019, she knew of 10 cases, she says. “Even when I’m not around I get a call,” Mciteka says. “I say: okay, I’m far but let me see what I can do.”
In Kenya, the issue of abandoned newborns is not new. Last year, The Telegraph and The Fuller Project reported on a volunteer clean-up team, Komb Green Solutions, who had uncovered nine foetuses and babies in as many months while clearing one section of the Nairobi river of plastic, sewage and needles.
The river is just one place the babies are found: news of infants discovered in dustbins or discarded by the roadside hits headlines with unsettling frequency. But without a national centralised data system to keep track of the total, many cases go unreported.
Work by women like Mciteka offers a small window into the scale of the problem. In Kenya, abortion is illegal unless a woman’s life or health is in danger and almost two thirds of pregnancies among adolescent women aged 15-19 are unintended each year, according to the Guttmacher Institute.

The 70-plus members of the Komb Green Solutions team have also noted an uptick since the outbreak of Covid-19. They’ve stumbled on 34 cases in total so far – 13 of which they’ve found since May, according to Christopher Wairimu, the group’s secretary.
“Some of them were breathing,” adds Debra Ogollah, a 26-year-old volunteer, “but unfortunately they only lived some seconds.”
The team continue to bury the newborns they find— including eight sets of twins found over the course of one year—in an ever-growing makeshift grave nestled next to the river (local police have given them permission to do so, say the Komb team).

Several hours north of the capital, reports of the same issue are occurring across Nyeri County in central Kenya. In September, John Waruru, local assistant chief, rescued a newborn from a bush near the banks of the Gura River – the umbilical cord was still attached. On this occasion, the baby girl survived.
“I’m hearing of stories weekly,” says Nelly Munyasia, head of Reproductive Health Network Kenya (RHNK), a web of over 500 trained health professionals providing health services. “Initially it was just in Nairobi, but it seems to be spreading pretty fast across the country.”
Like many countries around the world, Kenya closed schools in March to help stem the spread of the virus. The move left some 18 million students with little to do for more than six months and restrictions on movement meant accessing contraceptives and reproductive health information became harder.
Related coverage: One-Fifth of Women Don’t Know if Abortion Is Illegal in Kenya, New Study Shows
The collapse of global medical supply chains earlier this year, meanwhile, is still causing knock-on delays and shortages for some clinics in Kenya. Several service providers in Munyasia’s network are reporting difficulty in accessing long-term contraceptive methods—such as hormonal implants and intrauterine devices (IUDs).
In Kenya, high rates of teenage pregnancy has long been an issue yet since mid-March, healthcare providers have repeatedly raised concerns about a spike during the pandemic.
Although comprehensive national data about the impact of Covid-19 is not yet available – and statistics can be patchy at best – community health organisations in informal settlements say, anecdotally, teenage pregnancies are soaring. And in the first seven months of 2020, the Ministry of Health noted a 35 per cent increase in the number of sexual and gender-based violence cases compared to the same period the previous year, particularly among girls aged between 10 and 17.
The Ministry of Health did not respond to The Fuller Project’s request for comment. During a September visit to Kibera, an informal settlement, one of its officials, Dr Mercy Mwangangi, acknowledged that “the same barriers that restrict sexual and reproductive health care during the most normal of circumstances still exist and are often magnified during the [coronavirus] crisis.”

Parallels can be drawn with the Ebola outbreak in West Africa from 2014 to 2016, where similar public health measures and safety protocols – such as quarantine, curfews, and school closures – put girls and women at higher risk of violence and rape, according to a study by the United Nations Development Programme. In parts of Sierra Leone, the rate of teenage pregnancy during the Ebola crisis increased by 65 per cent.
But a spike in unplanned pregnancies only tells half the story, says Elizabeth Okumu, a programme manager at the Trust for Indigenous Culture and Health (TICAH). “We can’t ignore the end result,” she says over the phone from Nairobi, “which is high numbers of unsafe abortions.”
Nearly 90 per cent of Kenyans live on less than £4 a day, and the cost of a safe abortion procedure, roughly £150, is out of reach for many women. Unsafe abortions are cheaper, but typically involve visiting backstreet quacks who prescribe a concoction of dangerous – and sometimes lethal – chemicals. There is little support or aftercare and young women are frequently left to fend for themselves.
“We’re talking about people who really can’t afford it,” continues Okumu. “And seven months into [the pandemic], it makes sense. The timing fits. Doctors want a safe abortion, which is typically done between one and three months. In that stage, there’s no foetus. When we see foetuses in the community, we know it’s the work of quack doctors.”
“It’s like you’re carrying a burden.”
— Ashura Mciteka, mother and trained health volunteer
Back in Dandora, Mciteka quietly covered the aborted baby with an old cloth. She informed the local area chief, who in turn called the police to deal with the situation. When a foetus or newborn is found, there is no official process – sometimes the local chief or police help, but often it falls to community members like Mciteka to arrange a burial (it’s a different situation altogether if the child is still alive).
The heaviness is taking its toll, says Mciteka, who earlier this year founded a 15-member community-based organisation to try and help solve the issue. She feels stressed and worn down. “It’s like you’re carrying a burden,” she begins. “I’m a mother of three and I have two girls…I’m worried we might lose a lot of girls.”
Her fears are not unfounded. In Dandora, at least two teenagers have died during the pandemic due to abortion complications, according to Mciteka. And when, back in October, the Kenyan government announced schools would be allowed to partially reopen, she was concerned.
Teenagers still face a huge amount of stigma in Kenya when they become pregnant before marriage – and in some schools girls are required to take mandatory pregnancy tests. Mciteka thought she might see an increase in unsafe abortions the weekend before classrooms swung back into action. Instead, one Saturday night last month, a 13-year-old girl hung herself, she says.

“She left a note,” says Mciteka, “telling her mother she’s very sorry. The boyfriend, the father, said he can’t help. Did she [not have] someone to talk to? Did she feel like being pregnant was the end of her life?”
For several weeks after finding the foetus, Mciteka’s daughter, Ella, didn’t leave their home. She only wanted to play inside. Since then, things have improved—she’s ventured past the front door but doesn’t wander far.
As a mother, it’s painful for Mciteka to watch something so dark take hold so close to home—but it’s also part of the reason why she can’t quit. “You see, I’m a Muslim, even my religion doesn’t support safe abortion. But if we don’t, how will my kids turn out? The girls in the community? We need to talk about it. I won’t stop talking about it.”
When the coronavirus struck, hospitals around the world faced a crisis like no other. The knock-on effect is likely to be as catastrophic, with delays to cancer, heart and stroke services as well as patients avoiding treatment altogether in a bid to stay away from Covid-19 hotspots.
We’re already seeing the impact: Globally, millions of women have missed breast cancer screening appointments because of paused services during the height of the pandemic in March and April. This means thousands of cancer cases could lie undetected and the diagnosis delayed, say breast cancer charities.
In Kenya, where breast cancer is the most common type of the disease, the picture is equally alarming. Across the country, the uptake of cancer screening services when it’s offered is eye-wateringly low.
Last year, only 1% of eligible women were screened using mammography, the X-ray test used to spot cancers at breast screenings, despite equipment being available in most county referral hospitals (cost, awareness and enough knowledge to operate the machine all play a role). Only a quarter of women aged 14 to 49 say they have conducted a self-breast examination, and 14%t have had a doctor or healthcare provider carry one out, according to the Kenya Demographic and Health 2014 survey.
Advanced stages
And this was before the pandemic. Now, the number of women receiving check-ups or screenings is even lower, says Dr. Miriam Mutebi, a breast surgical oncologist and Assistant Professor of Surgery at Aga Khan University Hospital. When more than half of cancer patients in Kenya are diagnosed at advanced stages — and there’s fewer than 50 oncologists for a population of 54 million — it becomes all the more important for women to be able to spot any early warning signs.
We spoke to Dr. Mutebi about the challenges she’s seeing and why now, more than ever, a breast self-examination might just save your life.
What impact has the pandemic had on breast cancer screenings and treatment?
Unfortunately, we’ve taken a hit. During the lockdown period, many patients couldn’t travel into the city or were a little stranded in terms of accessing care or treatments. Now, I’m seeing a number of people who found a lump back in February or March but are only just coming into the hospital now.
Initially, there was so much uncertainty and confusion around the Covid-19 rules. I think the message that a lot of people received was; you go to the hospital, you get the coronavirus, you die. A lot of people just thought: “I’d rather wait.” Towards the end of July, patients slowly started to come back, but it’s worrisome. In the oncology community, we talk a lot about how COVID-19 has pretty much stopped everything except cancer — the cancer cells are still growing.
What kinds of cases are you seeing?
It’s a mix. We’re still seeing people who find a lump and come in within days or weeks. But quite a number of patients are coming in when the disease is more advanced, and they need something called neoadjuvant chemotherapy upfront, which is used to try and shrink the tumor ahead of surgery. I’m also seeing more and more cases where the disease has already spread to different areas of the body.
This trend is unfortunately likely to continue, especially with a potential second wave. People are still concerned, and again not traveling to Nairobi and other major towns where most of the main breast cancer services are located. For patients who live outside the capital and have received a diagnosis, I try to redirect them to the closest healthcare facility where they can get treatment.
You mention redirecting women — what are some of the barriers to accessing treatment?
Pre-COVID, one big barrier was that patients would need to routinely travel several hours to access radiotherapy at the main referral hospital in Nairobi. And radiotherapy isn’t a one-off. You’ll likely need at least three to four weeks’ worth of treatment and you need to pay for accommodation in a strange city. Quite a number of people say, “you know what, I can’t afford this.” If we’re able to bring these services closer to patients, that’s a huge win.
Regarding screening and early detection, one of the major challenges we are trying to address is health-seeking behavior. Often the thinking is; ‘there’s nothing wrong with me, why would I go looking for trouble?’ The message we’ve been trying to get across is, paradoxically, if you go to a screening and find something, that’s the stage you want to catch it. Not only is it treatable then but potentially curable, too.
Socio-cultural barriers are also relevant. Women may rely on a partner or spouse for support and in some cases permission, to access care, which translates into delays in diagnosis and treatment.
And the cost, too?
Unfortunately, patients are still having to pay out of pocket. The National Hospital Insurance Fund (NHIF) helps to cover some of the care and treatment fees, but it currently doesn’t stretch to mammography, which can cost between Sh1,500 and Sh6,500. That’s a huge sum for lots of people and means the cost of screening for and treating cancer remains out of reach for many households in Kenya.
The National Cancer Control Program (NCCP) has just started to disseminate country specific screening and early detection guidelines. But there is no established national breast cancer screening program — and a lot of what we do is opportunistic screening.
During October’s Breast Cancer Awareness month, for example, extra screenings are often available and there’s an uptick in women going for check-ups. It helps that most of the major hospitals in Nairobi will drop their mammogram prices during this month, and NGOs will offer free or subsidized clinical breast exams or other screening services.
Screening is not an end point in itself. It’s what happens next that counts. It would be incredibly cruel to tell women: “we’ve found a concerning lump — you figure out what to do next.” Screening and early detection must go hand-in-hand with strengthening health systems to better support the entire spectrum of diagnosis, treatment and survival rate of cancer patients.
Does this uptick in awareness reach women across the country?
No, this represents a very small fraction of the population. The average woman in the rest of Kenya is not necessarily going to be like; “hang on, I need to get my breasts checked.” That’s why it’s critical to strengthen the outreach for these screening and early detection services on a primary health care level — people should be able to access these services without traveling to a large hospital or an urban area. Any woman visiting her local health centre for an antenatal check, or family planning clinic, should ideally be able to have a clinical breast exam and discuss breast awareness with a trained nurse or healthcare provider.
Why is it important for women to be checking their own breasts?
A lot of referrals come from women themselves – they’ve detected a lump and decided to get it checked out. The self-breast exam is part of a wider breast awareness strategy — being aware of your breasts and any change — and it’s definitely one of the tools that will aid in early detection. The earlier the condition is found, the better the chance of surviving it (and you’re less likely to need to have your entire breast removed). We want to give women the tools to be aware of their breasts and empower them to take charge of their own health.
How to do a breast self-exam in 6 easy steps
by Dr. Miriam Mutebi
Look
2. Check for any skin changes; any lumps, swelling, dimpling or thickening. Check for any changes in the nipple; discharge or a nipple that looks like it’s getting inverted/being pulled inwards (and wasn’t before) should raise alarm bells. (Sarah Ijangolet/The Fuller Project)
Move


Feel

As a young girl, Amina Ahmed watched her grandmother, Hauwa’u Musa, guide women through labours that lasted for hours. And, just like her grandmother, she spent years perfecting her own midwifery skills. She did this in homes across Kano, the largest city in northern Nigeria.
“She taught me everything I know,” says Ahmed over the phone from her home. “Now, any woman who is pregnant, they call me.”
But Ahmed’s work doesn’t end there. After a woman gives birth, the 37-year-old then accompanies the family to a local healthcare facility. There, a nurse gives the newborn two droplets of the polio vaccine. It’s a small but life-saving action. Polio is a highly infectious viral disease that can cause paralysis and death, particularly in children under five.
On 25th August, the World Health Organization (WHO) declared the African continent free from wild polio, the crowning victory of the largest internationally coordinated public health effort in history. The success of the campaign, which lasted three decades, was described by the WHO’s Director-General Tedros Adhanom Ghebreyesus as “one of the greatest public health achievements” of our time.
Experts say the eradication of wild polio in Africa indicates just how challenging it can be to curb or eliminate an infectious disease: a lesson they believe has become increasingly apparent as the world works to combat the spread of COVID-19. Already, ten months into the devastating coronavirus pandemic, the virus has infected over 40 million people globally and taken over one million people’s lives. Now, as countries race to produce a safe COVID-19 vaccine, the question remains: How do governments and the wider medical community successfully immunise the entire world?
Harnessing the power of women
The answer might just lie with women, who played an enormous role in eradicating wild polio across Africa. World leaders, scientists and civil society can more effectively respond to COVID-19 by harnessing the power of women in local communities globally, says Sona Bari, a polio expert with the WHO.
Decades ago, wild polio paralysed more than 75,000 children across the African continent every year. In 2012, rates in Nigeria — the continent’s most populated country — accounted for more than half of the cases worldwide. While Europe has been polio-free since 2002, and the United States since 1979, wild polio remained active in parts of Africa until August of this year, as well as in Afghanistan and Pakistan, where spikes continue to this day.
Each year, a version of the virus known as vaccine-derived polio still circulates across Africa. It’s caused by a mutant strain of the oral polio vaccine. It poses a threat but rates are low – this year, 172 cases and zero deaths have been reported in 14 countries – and occurs in areas where there are immunity gaps.
Still, without female health workers, it’s likely wild polio would be responsible for the continued deaths of thousands of children across Africa every year. Women like Ahmed were key: they built trust, helped deliver vaccinations, and ultimately eradicated the disease. Going door-to-door, hundreds of thousands of frontline workers administered, or helped to administer, the vaccine to an estimated 51 million Nigerian children in one month in 2019 alone – the vast majority of whom were women.
Building on trust
“They were able to do that because they were granted access to the home,” explains Bari. “In many communities, men would not be granted access.”
Much of Ahmed’s work involves convincing the new mothers’ husbands of the merits of vaccination – not only from polio but from tuberculosis, hepatitis and meningitis as well.
“I meet them for a dialogue,” says Ahmed, referring to those men who appear wary of vaccinations. “Many times they agree after a chat.”

Their hesitations are understandable. Misinformation about vaccines has long been a major barrier to immunisation efforts in the region. It’s largely responsible for the persistence of the disease in Afghanistan and Pakistan.
There are enormous risks associated with contracting wild polio. Despite that, fears about the vaccine’s safety run rampant prior to its eradication across Africa. That’s according to Professor Rose Leke, Chair of the WHO’s African Regional Certification Commission for Polio Eradication. In 2003, four states in northern Nigeria suspended their immunisation programmes after unsubstantiated claims that the polio vaccine was part of a U.S plot to make Muslim women infertile.
Dispelling misconception
Yet female healthcare workers traipsed between millions of households, group meetings and places of worship to distribute information – and dispel misconceptions – about both polio and the vaccine. The reason why the information was well received, says Alice Awuor-Oyuko, a Save the Children senior health advisor, was simple. The women lived and worked in their own communities, and weren’t seen as outsiders.
Ahmed says she believes a COVID-19 vaccine would be welcomed by her community, despite the misinformation that continues to cast a shadow over immunisation programmes, just as long as women like her are on hand to provide public information and education. “People trust me,” she says, “so I find it easy to convince them.”
Now, to combat misinformation in the Covid-era, this work will need to be replicated. When scientists succeed in developing a COVID-19 vaccine, rolling it out will be equally, if not more, challenging than taking on wild polio, experts say – and its success will likely also depend on women. Globally, women make up 70% of health-care workers and 80% of nurses in most regions, according to U.N. data. As a result, it will be women like Ahmed who will likely need to squash community conspiracy theories, says Awuor-Oyuko.
“If [female healthcare workers] don’t uptake the vaccine that will be a problem,” says Professor Helen Rees, Executive Director of the Wits Reproductive Health and HIV Institute at the University of the Witwatersrand in Johannesburg. “They’re the very people who are going to be the backbone of outreach programmes for other adults.”
They have their work cut out, adds Awuor-Oyuko. The push to produce a COVID-19 vaccine coincides with the rise of the anti-vaxxer movement across Europe and the United States. Meanwhile, on the African continent, centuries of colonialism, medical experimentation, and recent racist comments about the testing of COVID-19 vaccines on the African population have made many in the region particularly wary.
“People are afraid,” says Leke from WHO. “[People on social media] are telling Africans: Don’t take any vaccines; they’re coming to eliminate you.”
Protecting communities
When a vaccine will be ready is still anyone’s guess. The UK’s Oxford University is leading one of the most advanced of the major global programmes to find a vaccine, involving participants in the UK, Brazil and South Africa, with a related trial in India. Russia became the first country in the world, in August, to approve a vaccine, and has since developed a second one, though critics warn there has not been enough testing for this to be safe.
Even before one is available, female health workers like Ahmed are playing a central role in keeping their communities safe. In the early months of the pandemic, Ahmed initiated a health campaign aimed at educating families in her hometown on the importance of handwashing, social distancing and mask-wearing.
“I tell them COVID-19 is real and they must adhere to the rules,” she says. “Just like polio, going from house-to-house telling residents [about the current situation] will help immensely.”
Her work is critical: When a vaccine is eventually produced, it’s unlikely to be available to everyone. Medical professionals largely agree that the immediate priority will be vaccinating adults over fifty, as well as healthcare workers, care home employees and other vulnerable groups.
While the world waits, Ahmed will continue her life’s work. That is, educating and protecting her small community in Kano, a skill she learned at her grandmother’s knee. And, when the time does come to help deliver a lifesaving coronavirus vaccine, Ahmed will be first in line.
Exactly 13 months after first landing in Beirut, Lebanon, former domestic worker Esenam sat on a flight back to Ghana, carrying just the clothes she wore on her back.
Her first employer had confiscated most of the possessions she brought over with her; the second raped and tortured her. In June, with help from This Is Lebanon, a human rights organisation fighting labour exploitation, the 29-year-old found her way onto a repatriation flight.
“I don’t regret the decision to return because my life matters,” she says via WhatsApp, from her home in Accra, the capital of Ghana. “But I shouldn’t have done it. I should have stayed.”
In Lebanon, Esenam, who asked to be identified by her middle name out of fear of reprisal from her former employer, earned £150 a month, which she wired home to her three children.
As the coronavirus ravaged Beirut and the Lebanese economy imploded, Esenam’s employers became more abusive. She, like many other domestic workers, chose to return home – many more have been deported involuntarily.
The pandemic and resulting economic crises have led migrant workers around the world to return to their home countries in the tens of thousands.
Since mid-March, more than 30,000 Ethiopian workers have re-entered the country, according to the government. Domestic labourers – more than half of them women – across the Persian Gulf make up a significant chunk of those finding their way back, as well as those from other Arab countries, such as Lebanon and Jordan.
They may arrive safely, but their problems aren’t solved once the plane lands. Many will return to no job, no savings and face potentially long-lasting psychological scars.
Millions of migrant workers in the Middle East
Each year, millions of migrant workers flock to the Middle East and to parts of Africa in search of better-paid work. In the Arab world, many end up exploited as housekeepers or nannies. Under the controversial sponsorship system, a domestic worker’s residency status is linked to their job.
In many cases, they cannot quit, move jobs or leave the country without their employer’s consent, which leaves women particularly vulnerable. Employers often demand long hours and provide minimal food. It’s also not unusual for them to be physically and sexually abusive.
Some migrants have reported being mistreated and abused in detention centres in the countries where they were working, such as Kuwait and Saudi Arabia.
Last week, a Telegraph investigation revealed hundreds of Ethiopian migrants who were slated for deportation have been left to rot in disease-ridden conditions in Saudi Arabia.
Once home, the trauma continues.
“Women have often been through a lot,” says Hugo Genest, of International Organization for Migration (IOM) Ethiopia. “Many of them are suffering from post-traumatic stress disorder related to gender-based violence. If they have a baby as a result of rape, for instance, it can be particularly difficult.”
In Ethiopia, returnees are typically screened for vulnerability by IOM on arrival back in the country. Before the pandemic, those in need were provided with medical and counselling support at one of their transit centres. Now, upon arrival, migrants must go directly to one of the quarantine centres across the country for at least a week before they can go home.
Once settled, women are asked to sleep alone in rooms in adherence with social distancing rules, but they often refuse or ask to share a bed with a female friend who travelled with them. “They don’t trust what can happen at night,” says Mr Genest.
In the quarantine centres, IOM is providing initial mental health care for returnees and offers referrals to local organisations for particularly vulnerable migrants, such as survivors of trafficking. But countrywide there is often minimal availability to much-needed psychosocial services, and women can slip through the cracks. Without support, returnees risk developing severe mental health issues, say rights groups.
“It’s a real problem,” adds Mr Genest.
Increasing hostility amid COVID-19
Migrants also face increasing hostility as potential virus carriers. After being sexually harassed by her employer in Kuwait, 22-year-old Fetiya Sewinet left her job as a housekeeper – and the chance of recouping nine months of unpaid salary – in June. Back in Ethiopia, her family were happy to see her but were wary of her time spent in the quarantine centre – they feared she might infect them with the virus.
Two months in, her neighbours are still suspicious and avoid her. “They think I’m sick,” she says over the phone. “I feel quite bitter about it.”
The economic stigma of returning without money or savings can be equally difficult. Families, and occasionally whole communities, will often help finance the original journey abroad for workers who in turn send money home.
“People think: How can you go to Dubai, the city of gold, and come back with nothing?” explains Paul Adhoch, the executive director of Trace Kenya, a Mombasa-based counter-trafficking NGO. “And most won’t tell anyone what they went through. If you fall into depression, you’re even more stigmatised because now you’re a burden to the family.”
In Kenya, there is a government-backed referral mechanism to help support victims of trafficking, yet few know it exists, say rights groups. In reality, the Migrant Workers Forum, an informal network made up of 15 civil society organisations, including Trace Kenya, often steps in to offer help where they can. Between them, they cover shelter, medical assistance, psychosocial services and information on safe migration for workers across the country.
Economic empowerment is important for proper reintegration, says Mr Adhoch, but lack of funding is a challenge. Most workers return without a job to countries already struggling with high levels of unemployment. Months into a pandemic, the chances of finding work look particularly bleak.
“Most won’t tell anyone what they went through. If you fall into depression, you’re even more stigmatised because now you’re a burden to the family.”
Paul Adhoc, Trace Kenya
The lack of support can push some back into the arms of unscrupulous recruitment agencies.
Just weeks after arriving in Ghana, Esenam began planning her return to the Middle East. She’s in touch with an agent who says he can fly her to Dubai – if she can raise £765. So far, she has received no psychological support. “I fear,” she says, “but I need to go. Thanks to coronavirus, there is nothing left in Ghana. I’ll be okay this time because I’ll work as a cleaner in a restaurant – not a domestic worker.”
Where possible, Trace Kenya provides returnees with funds to keep them going in the short-term, or start a business in the longer-term. Of the 200 plus Kenyans assisted by the organisation last year, roughly 15 per cent received financial help, he says.
In Ethiopia, IOM is ensuring migrants return home safely after the quarantine period. They do cover the cost of further medical care, psychosocial support and new business ventures but this is usually on a case by case basis, says Genest, and again budget dependent.
“The fact is, it’s expensive,” says Phil Brewer, director of intelligence at Stop The Traffik. “Not every country can provide a high level of support to those who return. Even if the goodwill is there, it may be that system breaks down because the financial backing doesn’t exist to make a genuine difference.”
Left to figure it out by themselves
Many women are simply left to figure it out by themselves. Take Wanjuki, a 36-year-old Kenyan who until two weeks ago had been working 20-hour days as a domestic worker in Lebanon. Her employer frequently locked in her room for hours and was verbally abusive towards her.
After months of ignoring her pleas, her employer eventually covered the cost of the flight home. As she stepped off the plane in Nairobi, the Kenyan capital, a sense of calm washed over her.
It felt good to have her freedom, says Wanuji, who also asked to be identified by her middle name out of fear of further stigma. But with just £380 in savings, two young children to support single-handedly and no job prospects, a looming sense of fear is slowly trickling into her newfound peace.
“I had dreams,” she says via phone from her home in Kirinyaga, a forest-filled county situated at the foot of Mount Kenya. “I thought I would go to Lebanon, buy a piece of land and build a small house for my kids – now my dreams have shattered.”
For the second night in a row, a group of Kenyan women have slept on mattresses outside the Kenyan consulate in Beirut, Lebanon on concrete pavements littered with plastic bottles. As night fell, they held up a Kenyan flag and chanted, “we want to go home,” throwing trash and rocks at the locked gate protecting the building entrance.
The women are domestic workers who have lost their jobs, many of whom are now homeless. They are calling on the Kenyan government to fly them home immediately.
On Monday morning, an estimated 30 Kenyan women – at least three with children – took to the streets to protest. Many of the women say they have either been let go or have not found work since the ammonium nitrate blast devastated Beirut last week, killing scores of people and injuring thousands. They now have nowhere to live, along with some 300,000 others.
Attempted arrest
The women cannot afford money for meals, nor plane tickets home.
On Monday night, the army attempted to arrest one of the Kenyan women but a number of bystanders intervened and no arrests were made, according to rights groups on the ground.
“Us Kenyans, we are tired,” said Kathy, 31, a domestic worker who asked to use her first name because of visa issues.
“We’ve reached a point where we will die in Lebanon.”
“We don’t have any hope. Some of us have kids here. What will happen to us? I’m not able to pay my own rent, let alone a ticket home.”
In interviews with several women, many say they have either been deserted by their employers, lost their homes due to the blast or simply can’t afford the rent any longer due to both the ongoing economic crisis and COVID-19 pandemic.
“I just want to go home”
“The blast made me realize that you can die in this country anytime,” said Kathy, who has lived and worked in Beirut since 2017.
“The glass was falling on our heads. Half of the houses are gone. Thank God I survived but I’m very mad. I’m going crazy. I just want to go home.”
The group is calling on Kenya’s Honorary Consul in Lebanon, Sayed Chalouhi, and his assistant, Kassem Jaber, both Lebanese nationals, to help.
On Monday, Kathy said she asked Jaber about the cost of a repatriation flight. When she explained that she had no money, he replied that she could engage in sex work to cover the fee, according to Kathy.
Two women – one Kenyan, another from Tunisia in close contact with the group – verified Kathy’s story. After the Daily Nation reached out for comment, Jaber denied any allegation of wrongdoing.

In a WhatsApp message, he wrote: “As a consulate and as a person who represents the name of a country, we will never ask a girl to do such a thing, we are always here in this country trying our best to help those girls to go back home.”
“I understand their anger and their need to go back home, but I cannot understand when a girl come and accuse and spoil a name of a consulate that represents a government.”
Two weeks ago, CNN published a story detailing how both Chalouhi and Jaber allegedly physically and verbally assaulted Kenyan women seeking services at the outpost, including pressuring domestic workers to pursue sex work.
In response, the Kenyan government said they would dispatch a fact-finding mission to Beirut to “look into reports of mistreatment” at the country’s consulate.
This morning, the Kenyan Embassy in Kuwait said they are following up with the consulate in Lebanon, and that Kenyans stranded in Lebanon will soon be repatriated.
This has been confirmed by the International Domestic Workers Federation (IDWF), a global labour rights organization, who are in touch with Halima Mohamud, Kenya’s Ambassador to Kuwait, about the ongoing situation in Beirut.
“We have communicated to the Kenyans to register with the consulate and we are already trying to address their issue,” Mohamud told Nairobi News.
Devastating poverty
Volunteers and members of the public in Beirut have donated tents, mattresses, food and water to help sustain the Kenyan women.
On the ground, the women are being assisted by the IDWF, who is in conversation with the Kenyan government and Kenya Union of Domestic, Hotels, Educational Institutions, Hospitals and Allied Workers (Kudheiha) the domestic workers union, to speed up the process of repatriation.
They are also in talks with the International Organization for Migration (IOM) to accelerate repatriation of the most vulnerable, including potential survivors of trafficking.
The Arab country was already struggling with an unprecedented economic crisis, with thousands of families being pushed into devastating poverty.
The COVID-19 pandemic and last week’s explosion, which left a trail of destruction some 10 kilometres from the port, have only added to the misery.
No salaries
For the 250,000 migrant domestic workers in Lebanon, the vast majority of them women from African and Asian countries, life has become doubly hard.
For months, many domestic workers have lost jobs, received reduced or no salaries or were forced to work increasingly long hours as employers isolated at home due to the pandemic. In July, employers abandoned scores of Ethiopian women in front of their country’s consulate in Beirut, saying they could no longer pay them.
Under Lebanon’s controversial sponsorship system, women are routinely abused. Migrant workers cannot move to new jobs or leave the country without an employer’s permission.
Many workers rely heavily on their countries’ diplomatic missions for protection and to help figure out a way home in emergencies. But such missions, largely African and East and South Asian, have failed to provide aid.
Unclear fate
“The women are just sitting on the streets,” said Roula Seghaier, from IDWF, who is assisting the group with government negotiations.
“They have no money and a lot of them have no place to live. So when the consul demands that they leave, they have no place to leave to.”
“Their fate is unclear,” she added.
Another protester, 33-year-old Karen Wanjira, says she has not worked since the blast and is supporting her three children living back home in Nairobi. A part-time domestic worker, she has been forced to share a single room with six others who needed accommodation.
“I would like to say to the Kenyan government, humbly, please remember us,” said the single mother by phone.
“At least send a plane to take us home. You will save many lives.”


